TRAUMA REPORT 2020
Massage from Chief of BDMS Orthopedic and Trauma Care Network

According to the vision of our former president, Dr. Prasert Prasarttong-Osoth, MD, considered that BDMS, as a largest medical profession network of healthcare in Thailand should take more responsibility for the treatment of Thai citizens from road traffic accidents in order to reduce both death and disability from injury. Road traffic accidents lead to high mortality and morbidity rates, especially in young age groups. The BDMS’s vision is to develop trauma network nationwide with timely and highly efficiency trauma care to treat the injured patients. This vision was strengthened further to the Royal Phnom Penh Hospital which is one of the hospital network of BDMS in establishing a high standard trauma center to save lives for the people who live in Cambodia.
In response to the need for effective trauma care in Cambodia, Bangkok Dusit Medical Services Public Company Limited (BDMS) developed a Center of Excellence for Trauma as a mandate policy in September 2015. It has been 5 years to build up 11 BDMS Center of Excellence in trauma care located in different region of Thailand including Royal Phnom Penh Hospital which is located in Cambodia. Bangkok Dusit Medical Services (BDMS) guided by a strong collaboration with Hannover Medical School (MHH) in Germany, a pioneer of the Trauma system in Germany that started 50 years ago. The collaboration consisted of exchange of knowledge and training of our staff in Hannover to learn about trauma care and medical evacuation. From this know how it has elevated the quality of our facilities, services and practices, to become a Center of Excellence Network (CoE) in trauma care.
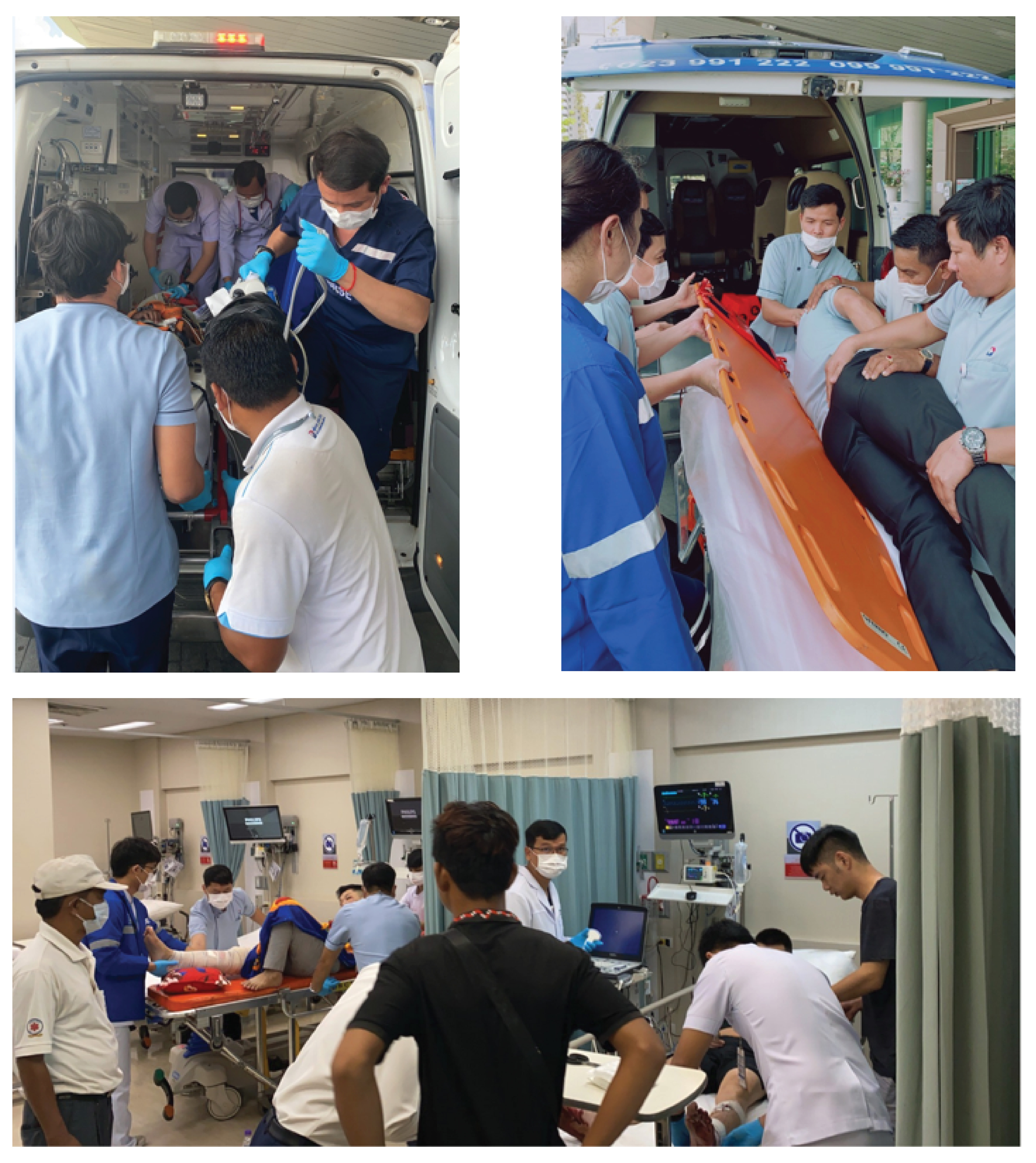
I strongly believe that the RPH trauma team has raised the standard of trauma care to the international level and proud to serve Cambodian community in this capacity. Cambodian will reassure that they have a top quality trauma center right here at home. To date, with 11 Centers of Excellence in BDMS Trauma care network, the system has integrated pre-hospital and facility-based trauma care systems to promptly respond to emergency cases, providing world-class healthcare services for Cambodian and international patients. There are 50 network hospitals around Thailand with differences in staff competency and level of care. In order to treat critical and serious trauma case there is a system for teleconsultation and a mobile surgical team upon request to support the treatment of patients in our hospital network.
This 2020 annual trauma report allows us to highlight our trauma outcomes and show significant improvement in productivity from the RPH trauma team They have work hard throughout the year with their commitment to be the best. I would like to express my sincere appreciation to all the team members and many supporting unit as well as the management team who focusing on the goal in supporting on our journey to improve the quality of trauma care of Cambodian community. Although there are many obstacles and restrictions in driving the trauma care service to the top tier I do hope that the situation will be better. I am pleased that RPH made such a good team and took the trauma care center to higher level with continuous improvement to accomplish our mission is to give the best possible care to our patients. With best wishes and kindest regards,
Suthorn Bavonratanavech, MD.

Chief of BDMS Orthopedic and Trauma Care Network
Table of contents
- Preface
- Message from the Hospital Director
- Message from the Trauma Director
- Summary
- Statistic of Trauma Patients
- Caring for the trauma patients
- Trauma Activity

Message from the Royal Phnom Penh Hospital Director

The Royal Phnom Penh Hospital is flagship hospital for the Royal Bangkok Hospital Group, operates in Phnom Penh, Kingdom of Cambodia, under close supervision of BDMS group, Thailand. The hospital had been accredited and re-accredited by the JCI since June 2017. The hospital supports systemic approach, vertical and horizontal co-ordination on trauma care by providing continuous medical training to trauma leaders at all level, enable them to do their best every day to ensure high quality care and patient safety. The hospital provides BLS training to every single hospital and ATLS to physician leadership in the trauma team. The hospital also supports clinical coordinator on trauma care, creating academic environment with BDMS group and worldwide academic network, to ensure compliance to the effective implementation of clinical trauma pathways.
The Royal Phnom Penh trauma care will continue to improve and trauma team will continue to work with local community to improve on awareness and prevention of trauma to ensure safe environment for all stakeholders, to attain healthy productive growth of knowledge and achieve sustainable economy of the Kingdom of Cambodia.
Be safe and well,
NARINTARA BOONJONGCHAROEN, MD.
HOSPITAL DIRECTOR
Message from the Royal Phnom Penh Trauma Director

In this year, 2020, it was the challenging year of ours.
The Royal Phnom Penh Hospital is the first JCI accredited and re-accredited hospital in Cambodia since 2017.
We committed for international standards in every inches in our hospital.
During pandemic of covid-19, there are many aspects that we need to realize the challenges of patient safety and staff safety in the same time.
As we known, the trauma patient need to receive immediate and properly care to save their life. That was call “time sensitive”. Any delay of treatment may lead to adverse effect, or even die.
In this era of severe pandemic disease, as covid-19, we achieved a new challenge to our team for serving the trauma patients without delayed and still protect our staff from covid-19 transmitted.
I would like to thanks Dr. Narintara as our superb hospital director for all the advices and always supportive, also thanks to Bangkok hospital and BDMS network to co-operate the work as the team.
The most important part of the Royal Phnom Penh Trauma Team that made all of this great work happen is all of the staff here, especially our hard work Assistant manager of center of excellence, Ms. Subpha Ongtip, all of them deserved the deepest thanks from me.
The challenging will continue and we always know that the room of improvement still, we need to work hard and even harder to improve ourselves to deliver the best services to everyone.
SUPALARP PASURAWANICH, MD.
RPH TRAUMA DIRECTOR
Summary
The Royal Phnom Penh hospital located in Phnom Penh city, Cambodia, was developed to be a trauma center level 3 and providing treatment services for trauma and emergency patients, and covering patient transportation service, resuscitation, surgery, and trauma intensive care.
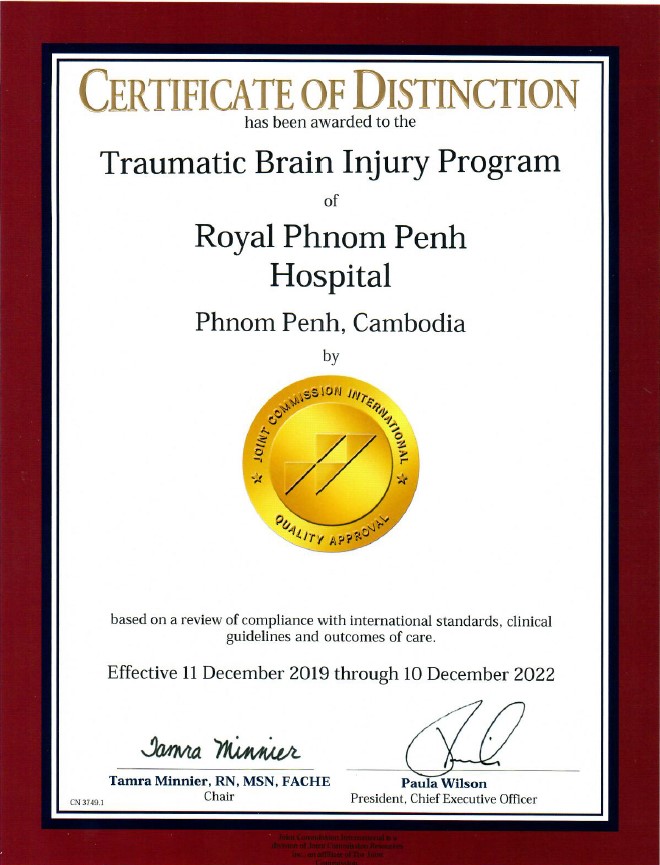
The hospital administrators have a cleared goal to achieve standardized treatments and patients safe, therefore, strive to improve quality continuously so we were the first hospital in Cambodia received the JCI accreditation in 2017. In the same year, we adopted the BDMS trauma algorithms, as well as training doctors and nurses about the trauma treatments and nursing cares to meet the target of patients safe and able to have an optimal quality of life while monitoring the trauma performance indicators to leverage the clinical outcomes. The results of trauma performance indicators were the reason that we have adopted trauma brain injury guidelines to serve the major trauma patients in Cambodia, since then, in 2019 we received the certification of the standard of treatment for patients with specific diseases-CCPC TBI (Clinical Care Program Certification of Traumatic Brain Injury), furthermore, we continue compliance with all of the JCI Hospital standards on an ongoing basis throughout the three-year accreditation so in 2020 we achieved the JCI reaccredited.
About the trauma and emergency services in RPH, in 2020 the total number of trauma patients who visited RPH was 1,044 decreased from last year due to COVID-19 pandemic affected. The 104 patients were transferred-in and 940 patients were walk-in. The highest age group of trauma patients was 25-44 years-old (36.30%). The total numbers of trauma in-patients were 194 patients decreased from last year and the average length of stay of trauma admission was 5.73 days.
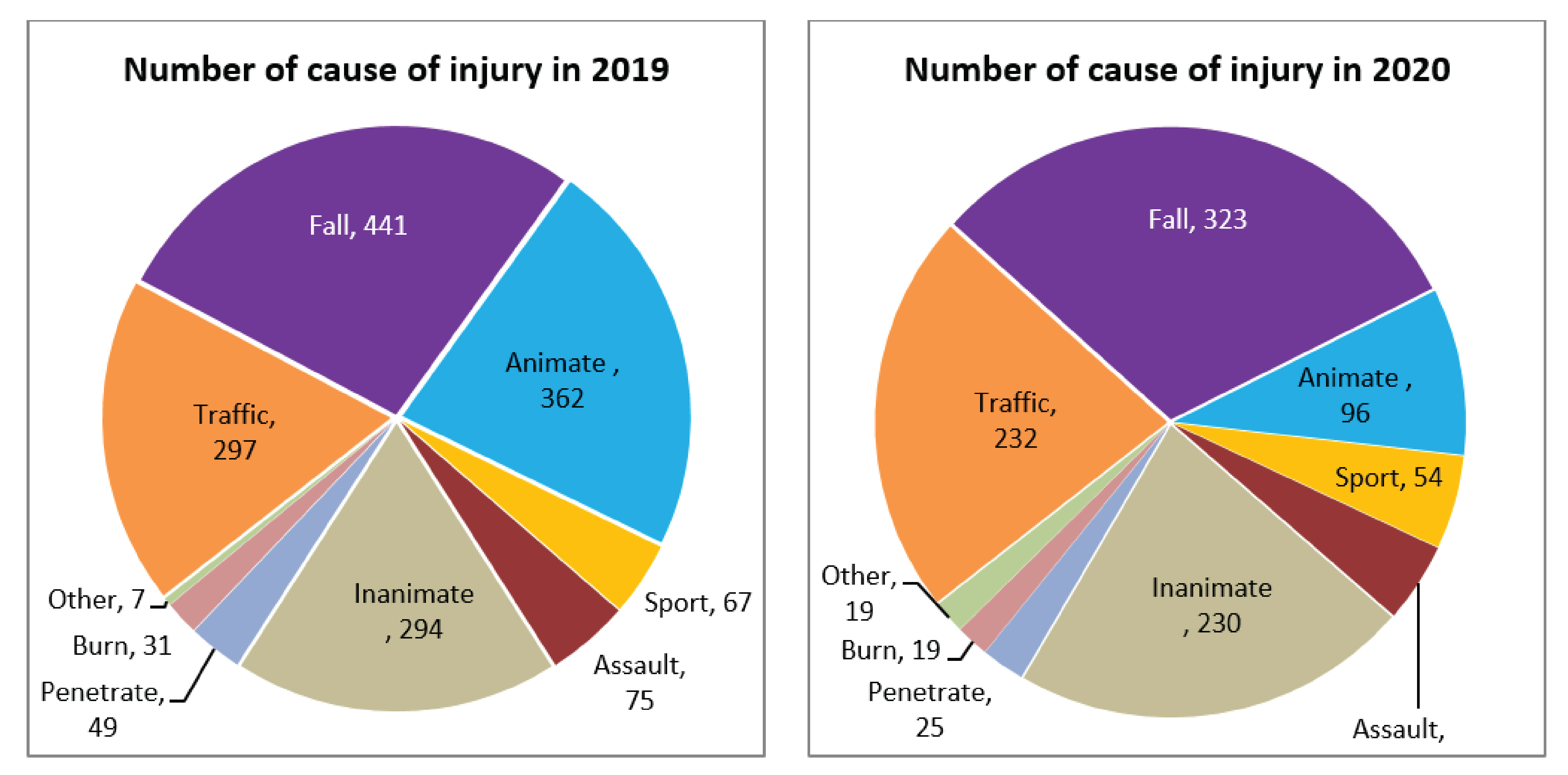
The most common cause of injury in 2020 still was fall (30.94%) followed by traffic accidents (22.22%) and inanimate injuries (22.03%). Therefore, the most significant community communication for the prevention of injury is how to prevent falls at home and drives safely.
SUBPHA ONGTIP
The assistant manager of center of excellence
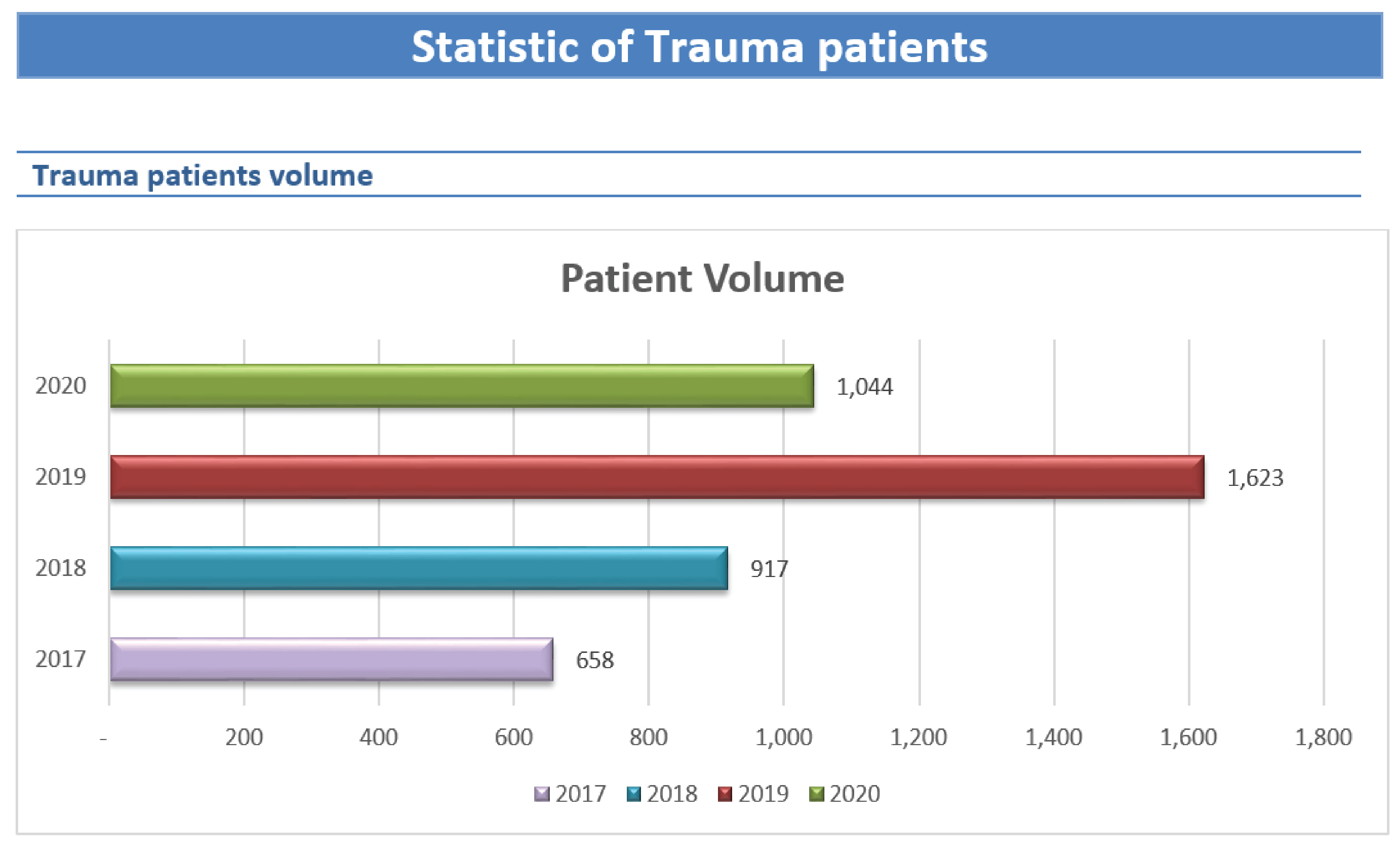
The number of trauma patients was increased respectively in 2018, 2019 but in 2020 it was decreased 35.67% from 2019.
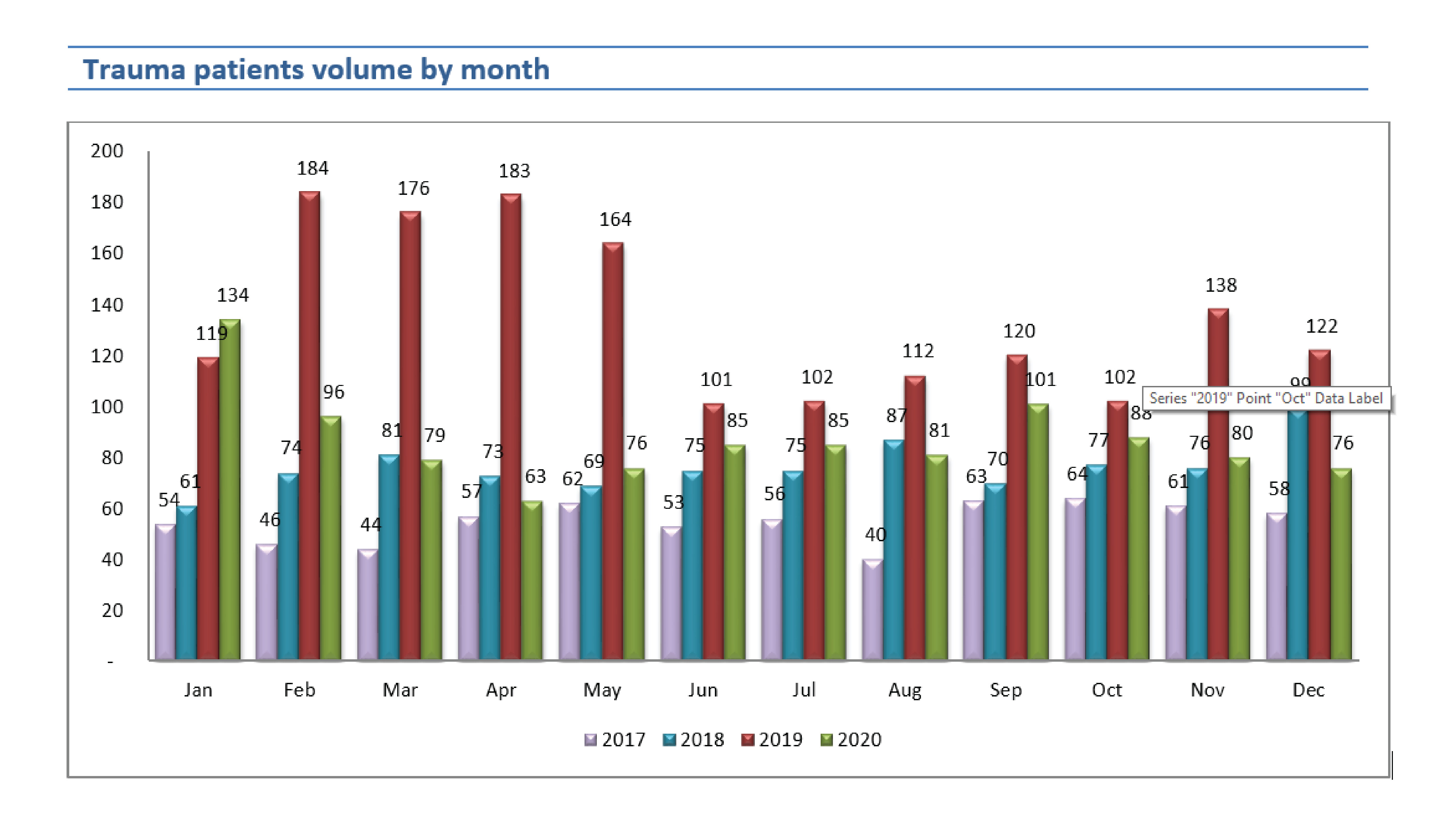
In 2020, the average number of trauma patients who came to RPH was 55, 76, 135, and 87 per month in 2017, 2018, 2019, and 2020.
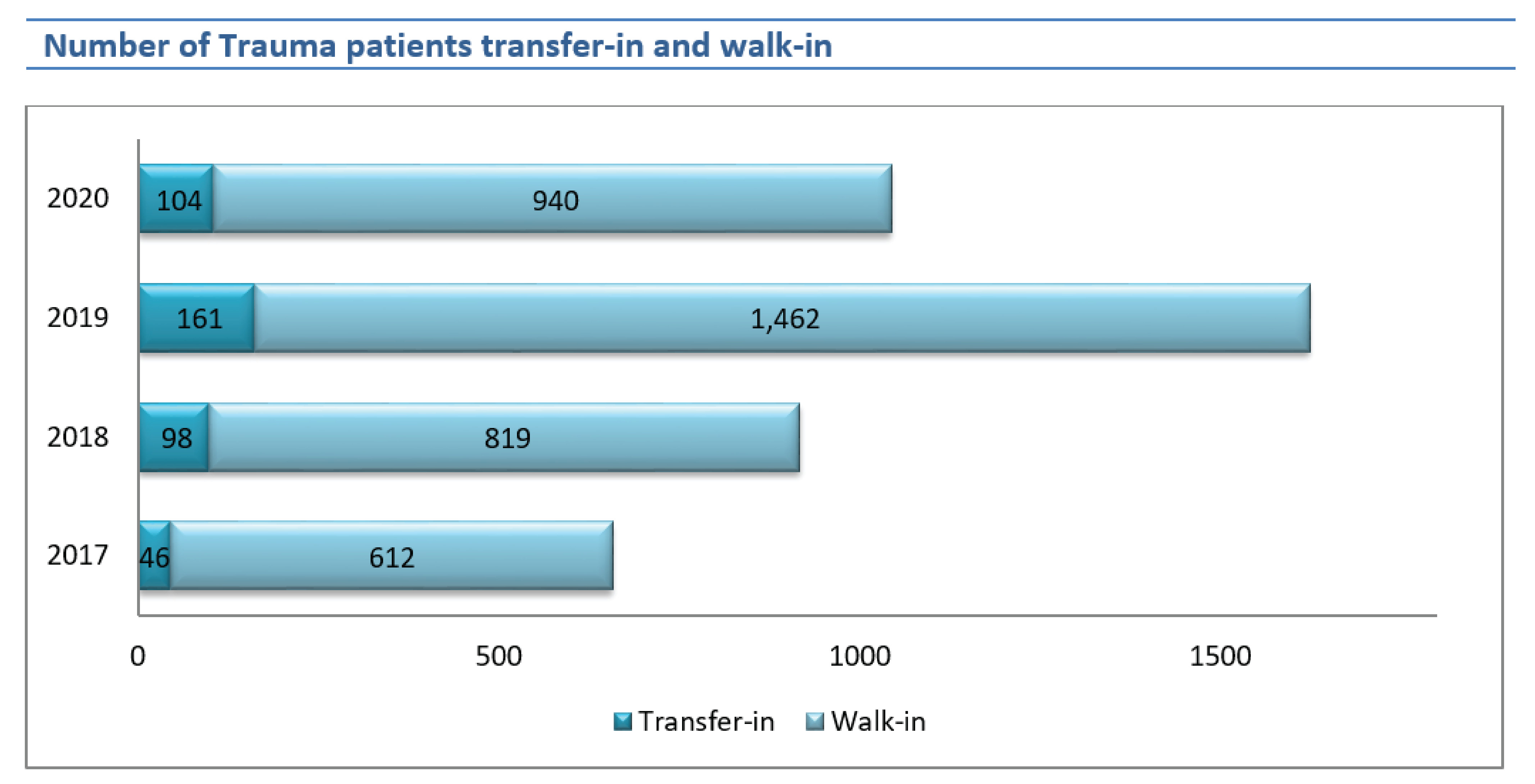
The number of trauma patients who were transfer-in to RPH increased in 2018 and 2019 but decreased 35.40% in 2020 by 161 to 104 cases.
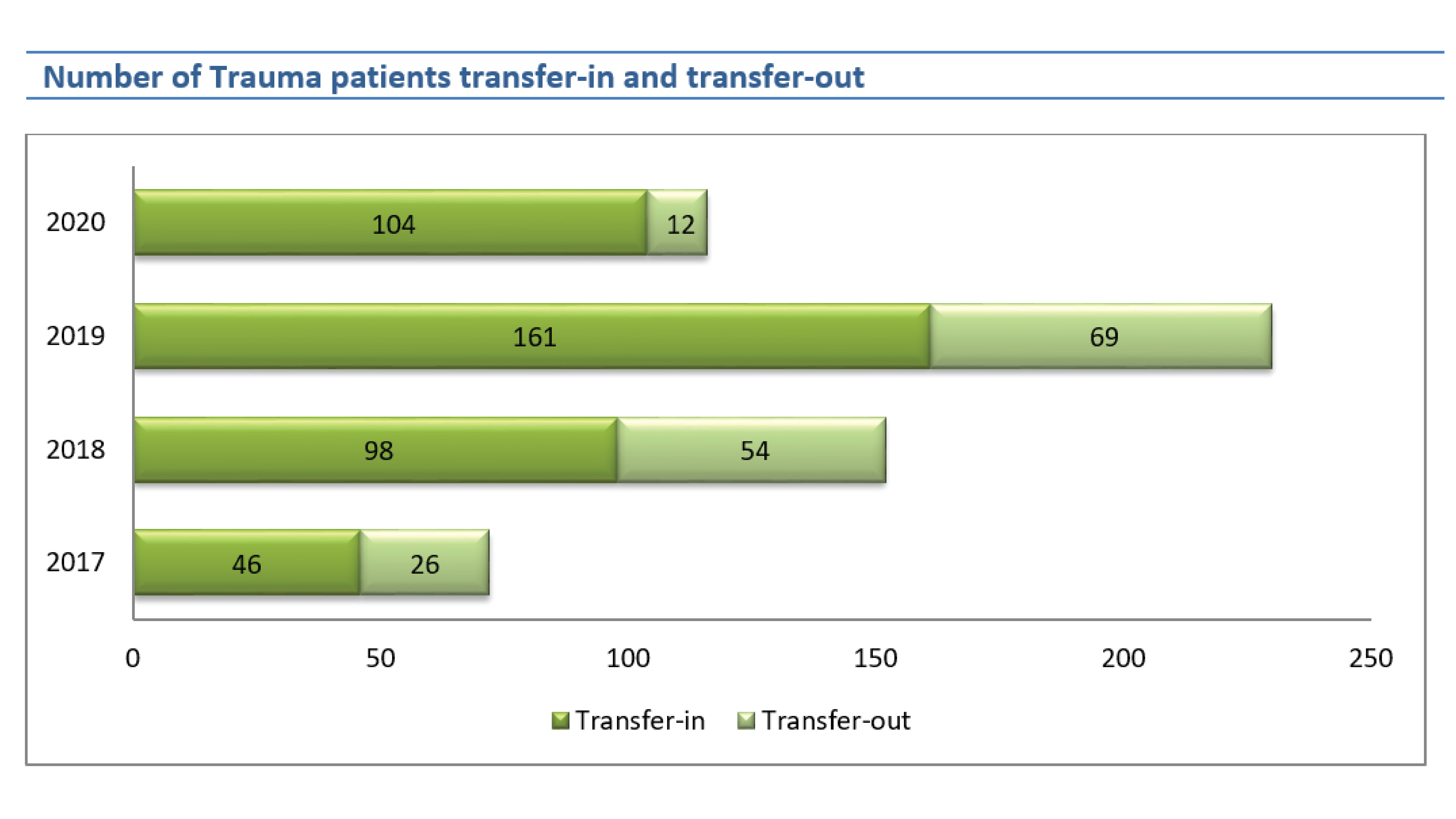
The number of trauma patients transfer-out increased in 2018, 2019 but in 2020 decreased 82.61% from 2019 by 69 to 12 cases. The ratio of transfer-in and transfer-out decreased from 1:0.57, 1:0.55, 1:0.43, and 1:0.12 in 2017, 2018, 2019, and 2020 respectively.
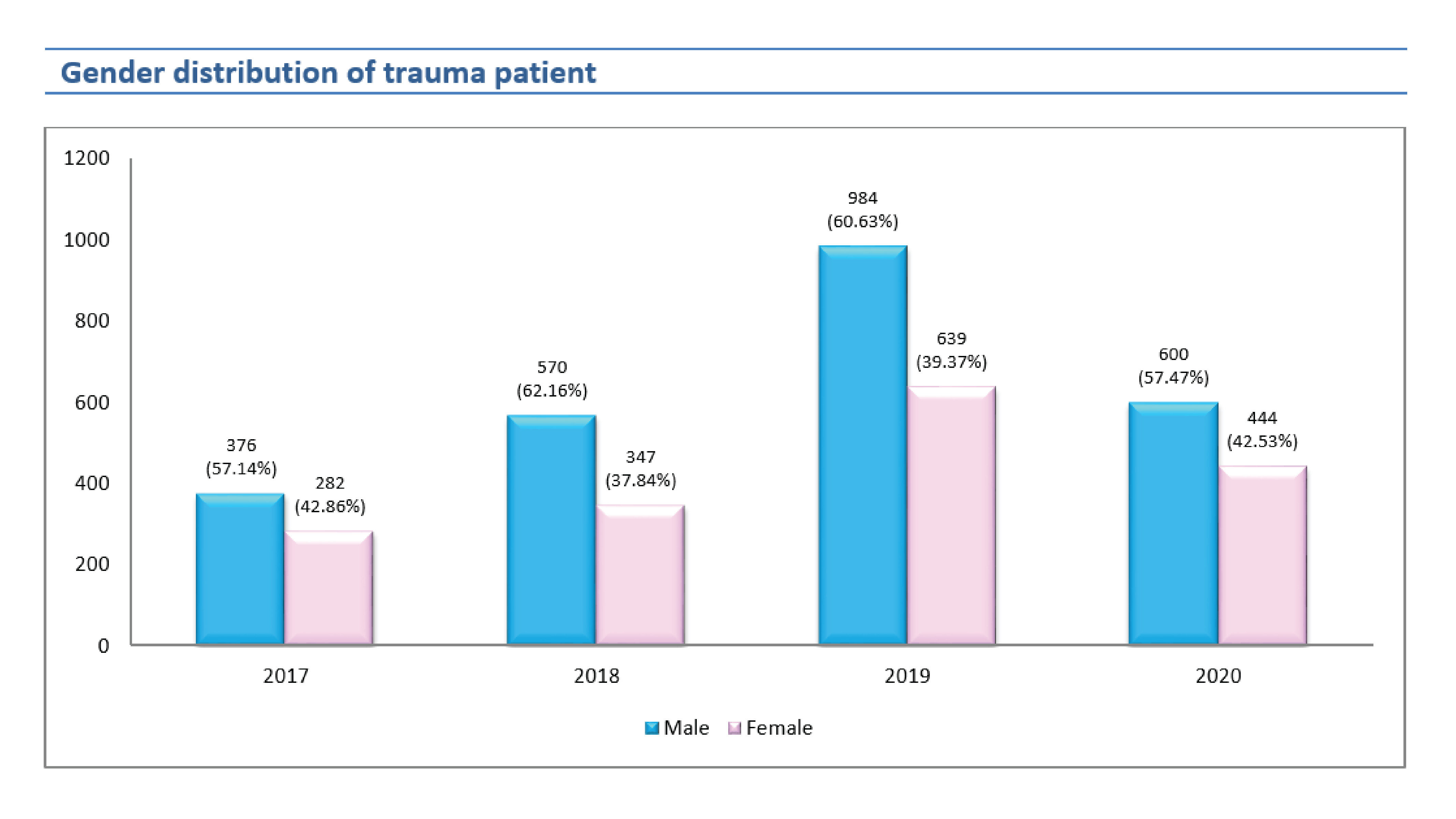
The number of trauma patients by gender showed the number of males has always been greater than females, but the number of female injuries tends to increase slightly.
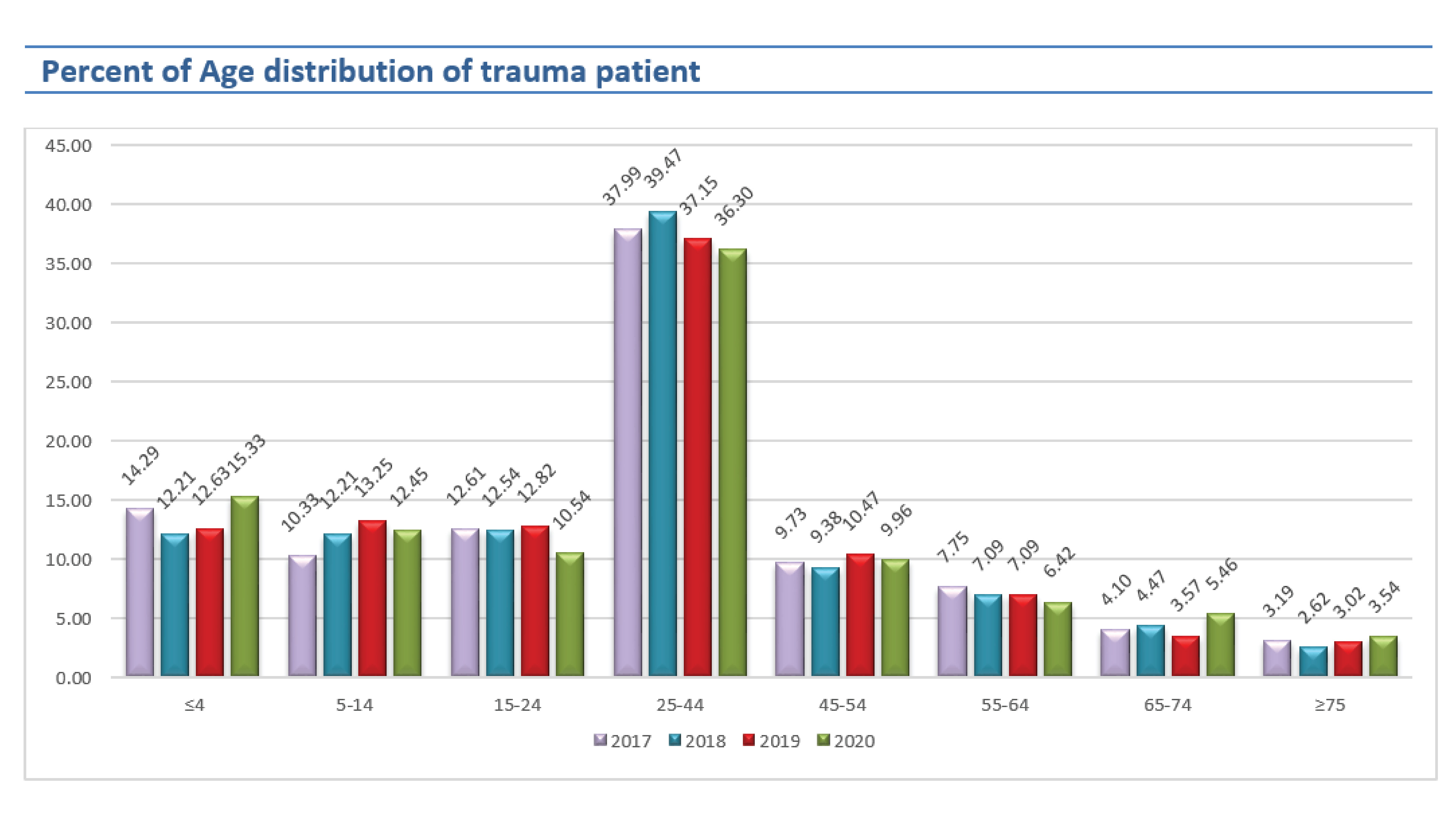
In 2020, the most trauma patient was 25-44 years old. The trend of trauma patients age ≤ 4 years old, age 65-74 years old, and ≥75 years old increased (17.58%, 34.55%, and 14.81% respectively).
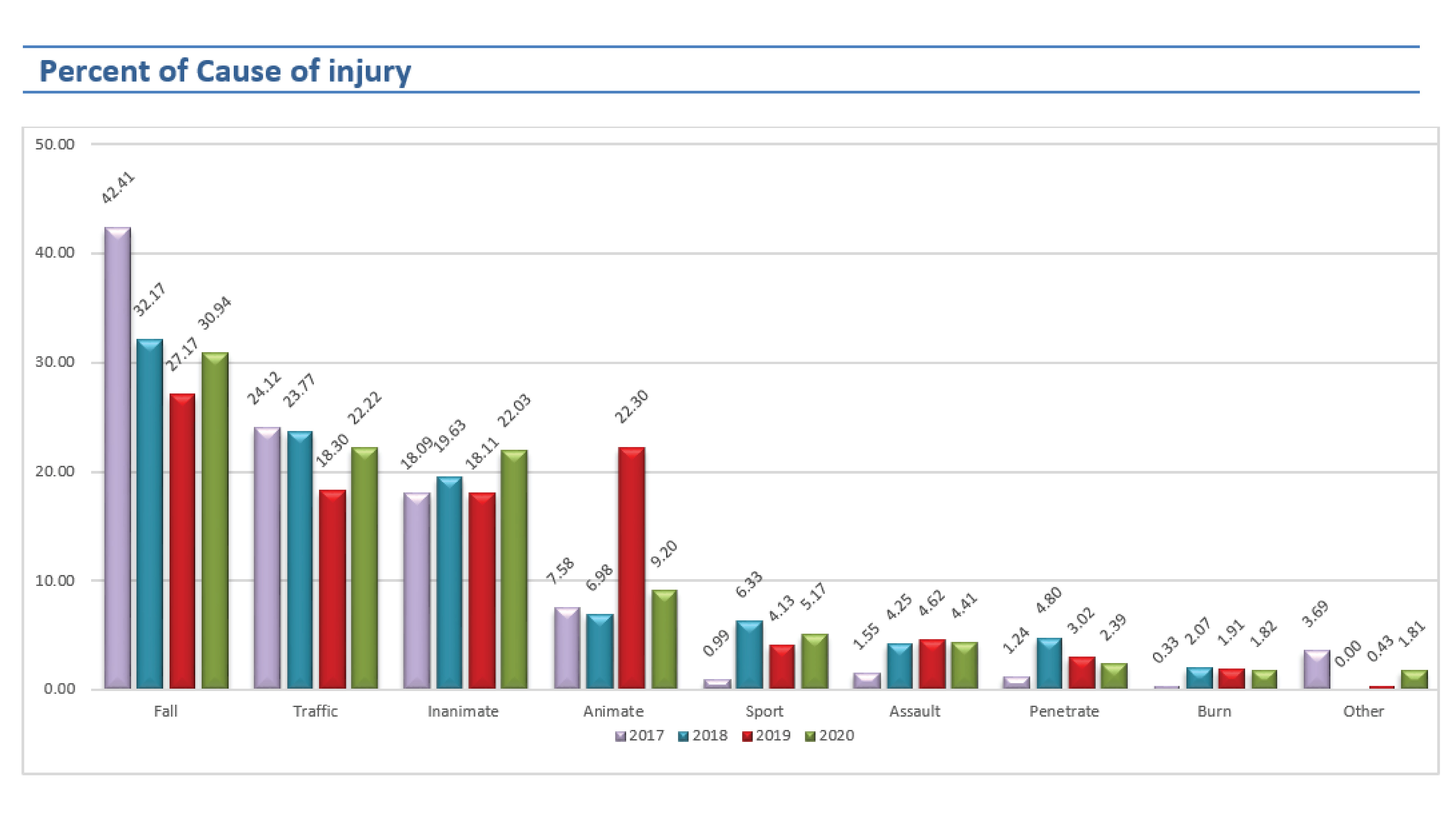
Slips, trips, and falls in the same level were the most common cause of injury but its trend slightly decreased. The percent of traffic accidents was nearly as same as the injury caused by inanimate.
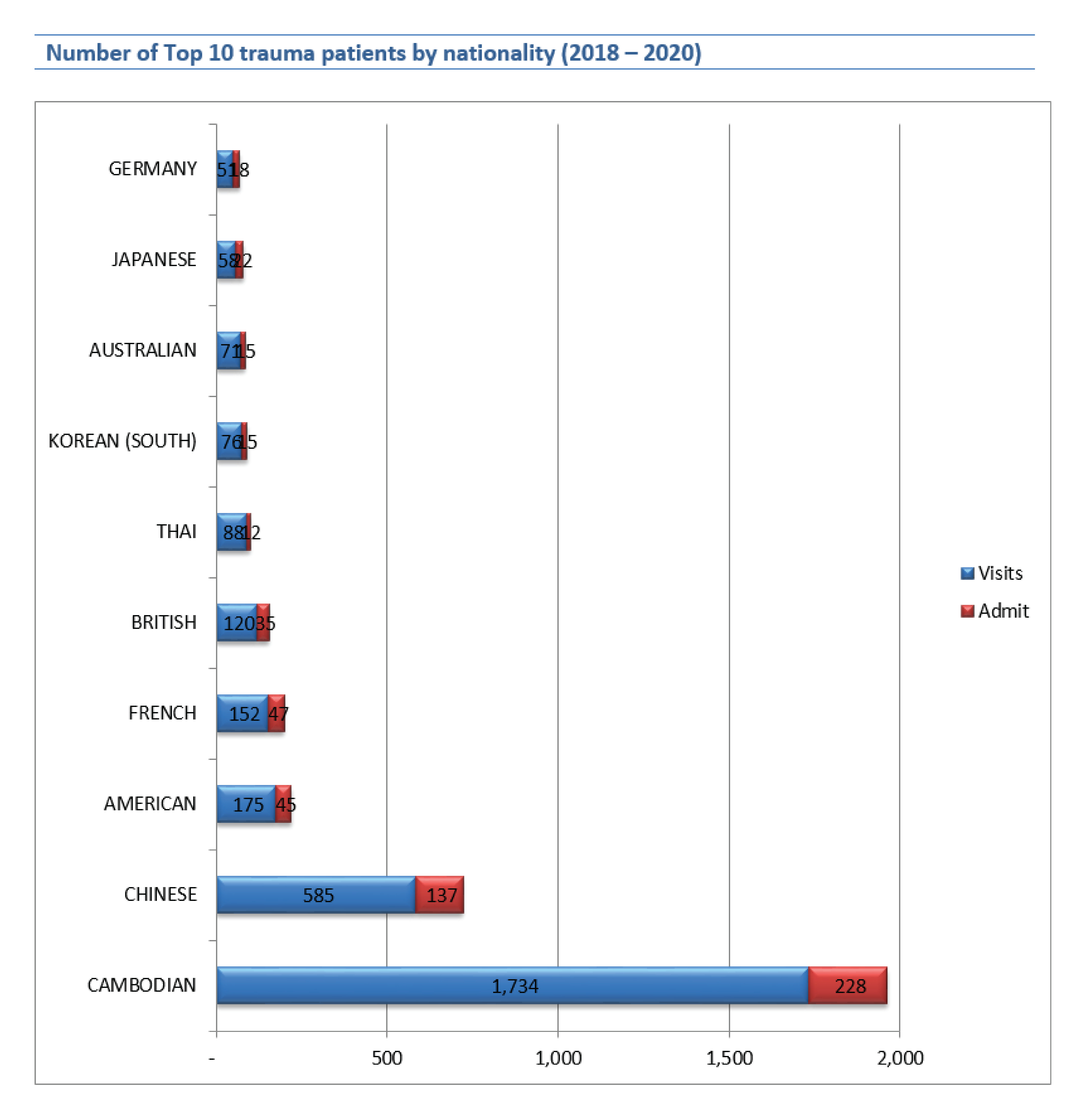
In 2018-2020, Most of the trauma patients are Cambodians while rising up with the number of Chinese trauma patients, and followed by American and French. The Chinese population increasing in Cambodia due to the growing investment by them. The number of international trauma patients in 2018, 2019, and 2020 were a bit different (510, 533, and 513) but local trauma patients increased in 2019 and dropped in 2020 (407, 769, and 531) that because the COVID-19 pandemic affected.
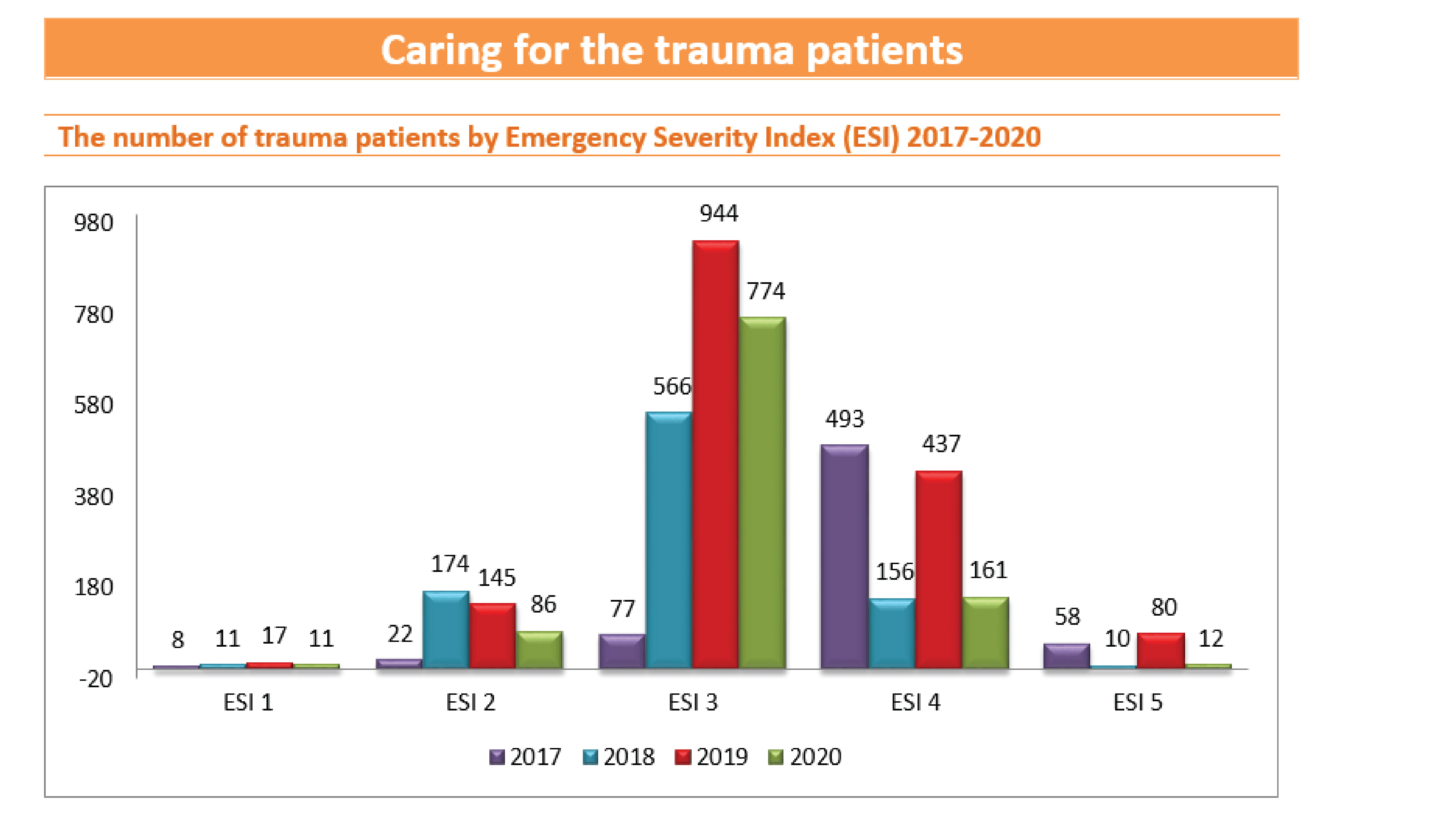
In 2020, the affected of the total number of trauma patients declined (1623 to 1044) so the number of trauma patients in all emergency severity index (ESI) levels declined as well, there were ESI 1 54.55%, ESI 2 68.20%, ESI 3 21.96%, ESI 4 171.63, and ESI 5 566.67%.
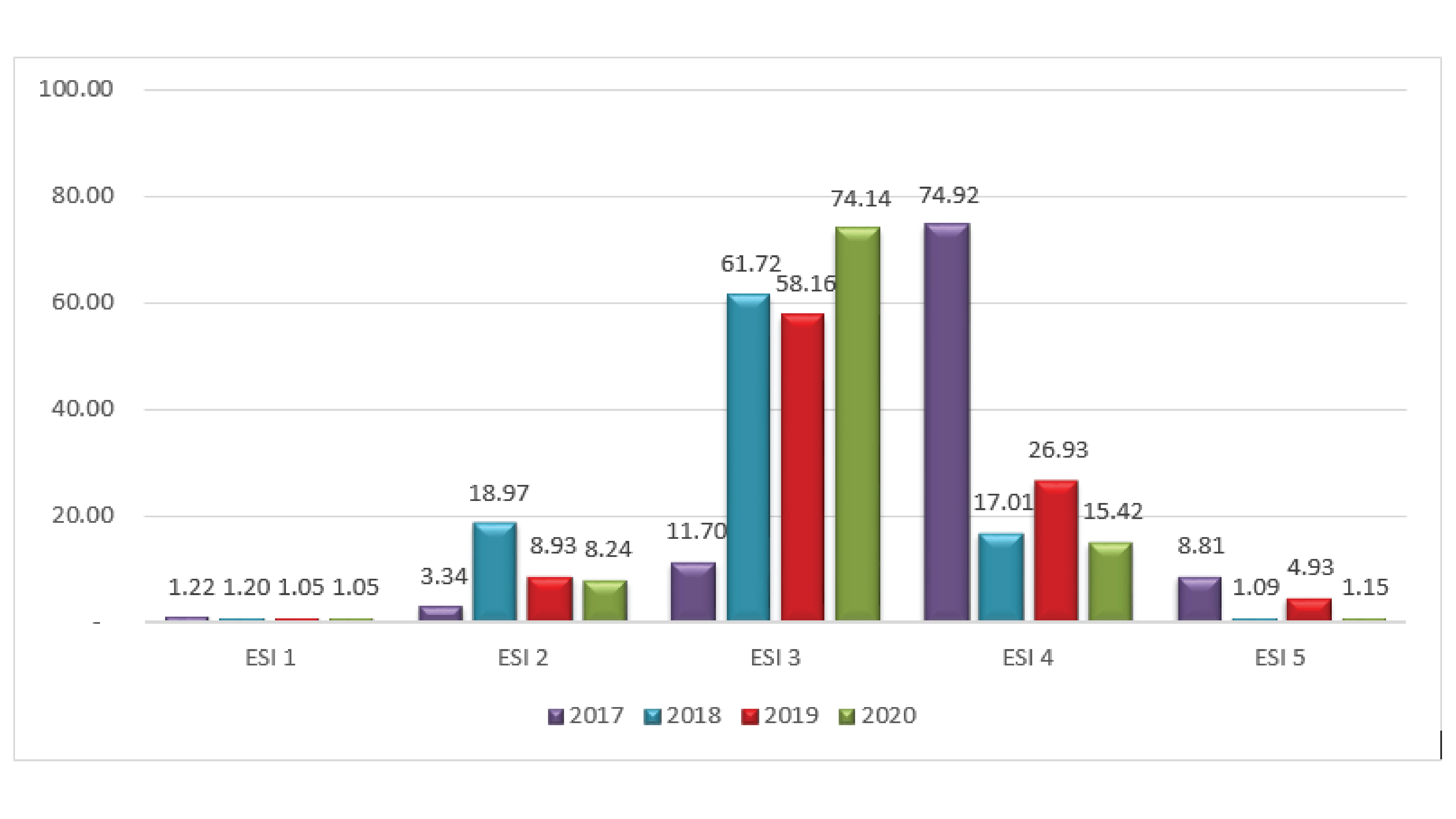
However, when comparing the percentage of patients in different emergency severity index found that ESI 1 and 2 were similar in 2020 and 2021. The ESI 3 greatly increased from 58.16% to 74.14%, on the other hand, the ESI 4 and 5 were dropped considerably.
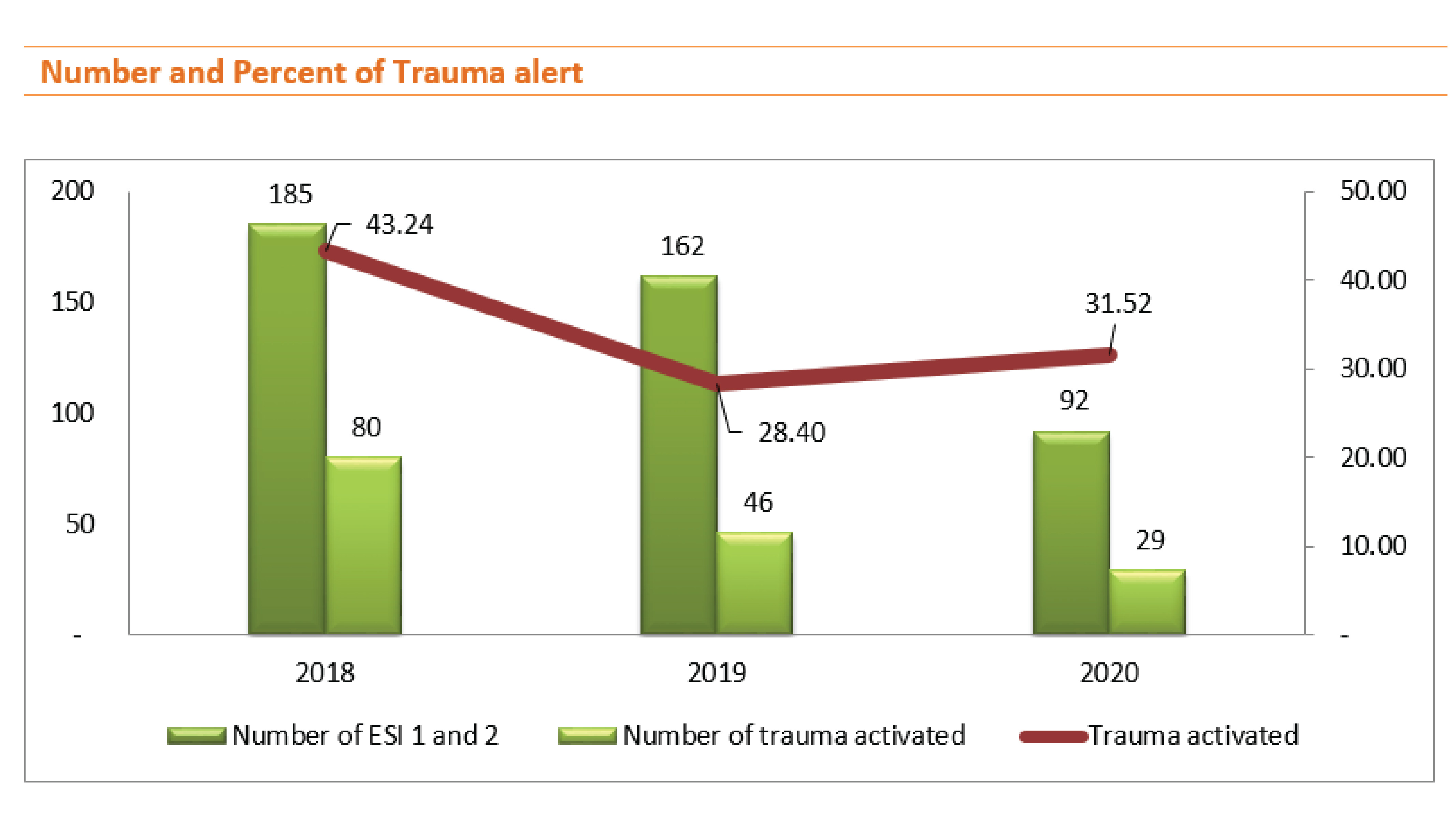
In 2017, the trauma alert code announcement was still under a learning curve, in 2018 we started collecting the trauma alert code announcement very intensively, and we have been looking for an opportunity to improve the trauma alert code declaration in accordance with the emergency severity index of the injury. In mid-2020, we created the trauma alert checklist to use in the emergency department, allowing more code declarations to be more accurate and relevant to the emergency severity index.
The percentage of announcing trauma alert code in trauma patients who were triaged as ESI 1 and 2 that met the criteria of trauma alert slightly increased from 28.40% (2019) to 31.52% (2020).
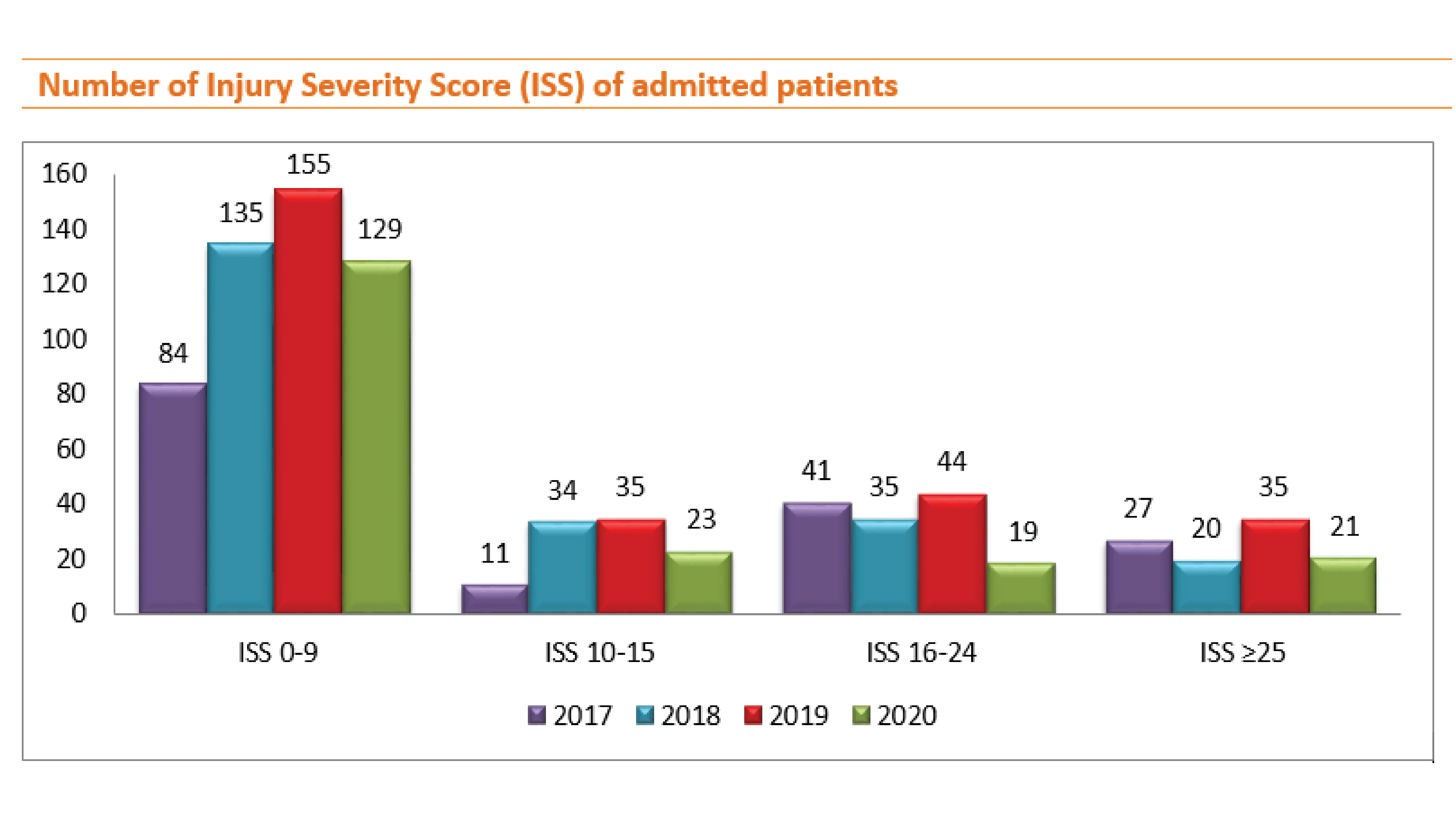
The number of trauma patients is increasing in 2018 and 2019, but in 2020, the number of trauma patients was declined for all groups of the emergency severity index, however, when comparing the percentage of inpatients, only ISS 0-9 was found to increased, the other groups decreased significantly.
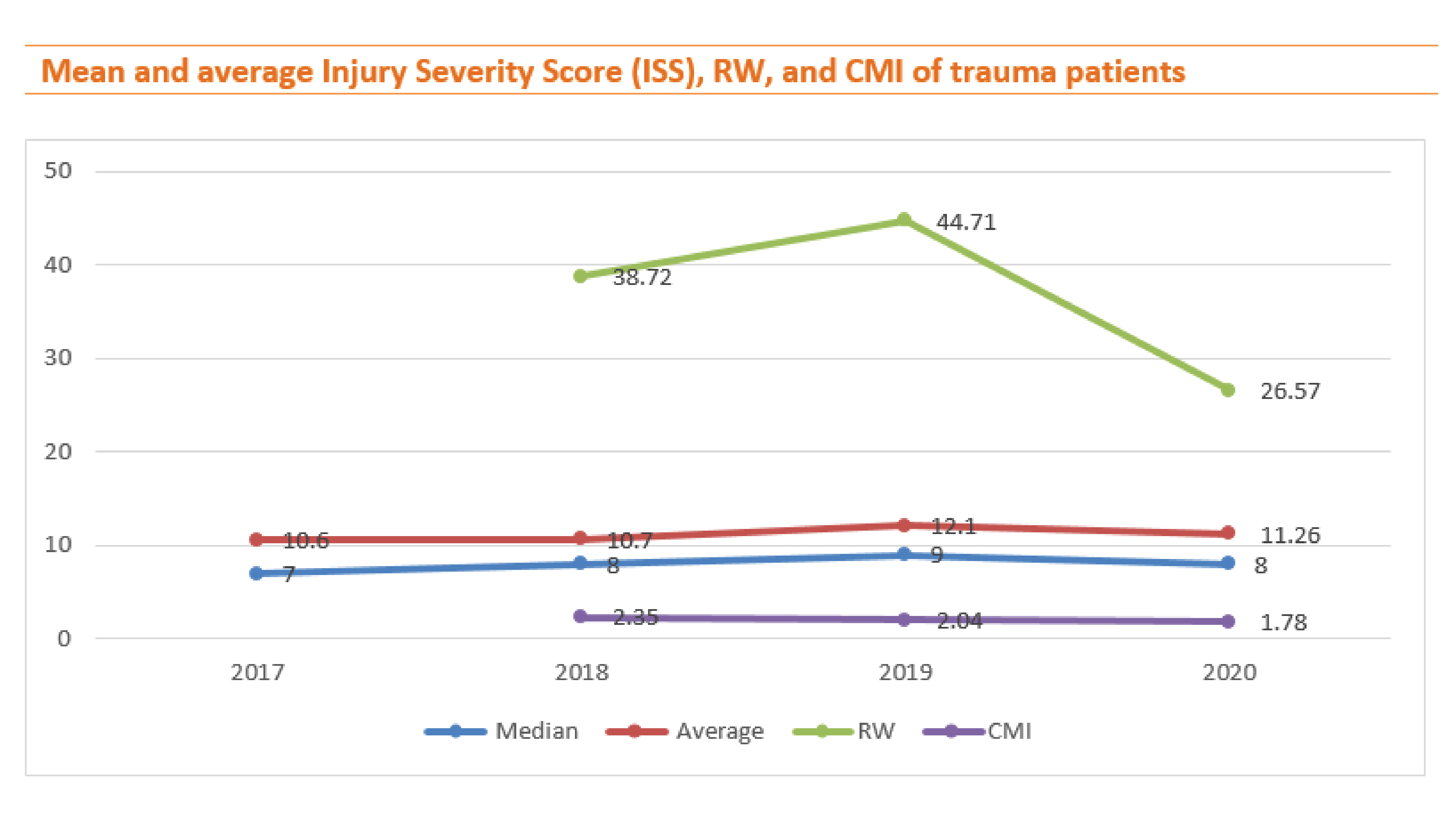
In 2020, the Injury Severity Index (ISS), Relative weight (RW), and Case mix index (CMI) declined but it is noting that the mean of ISS is only slightly lower if compared to the RW and CMI values. The CMI is a relative value assigned to a diagnosis-related group of patients in a medical care environment and relative weight means a numeric value that reflects the relative resource consumption for the DRG to which it is assigned. Therefore, in the trauma patients, we should pay more attention to CMI and RW as same as the ISS to achieve trauma targets.
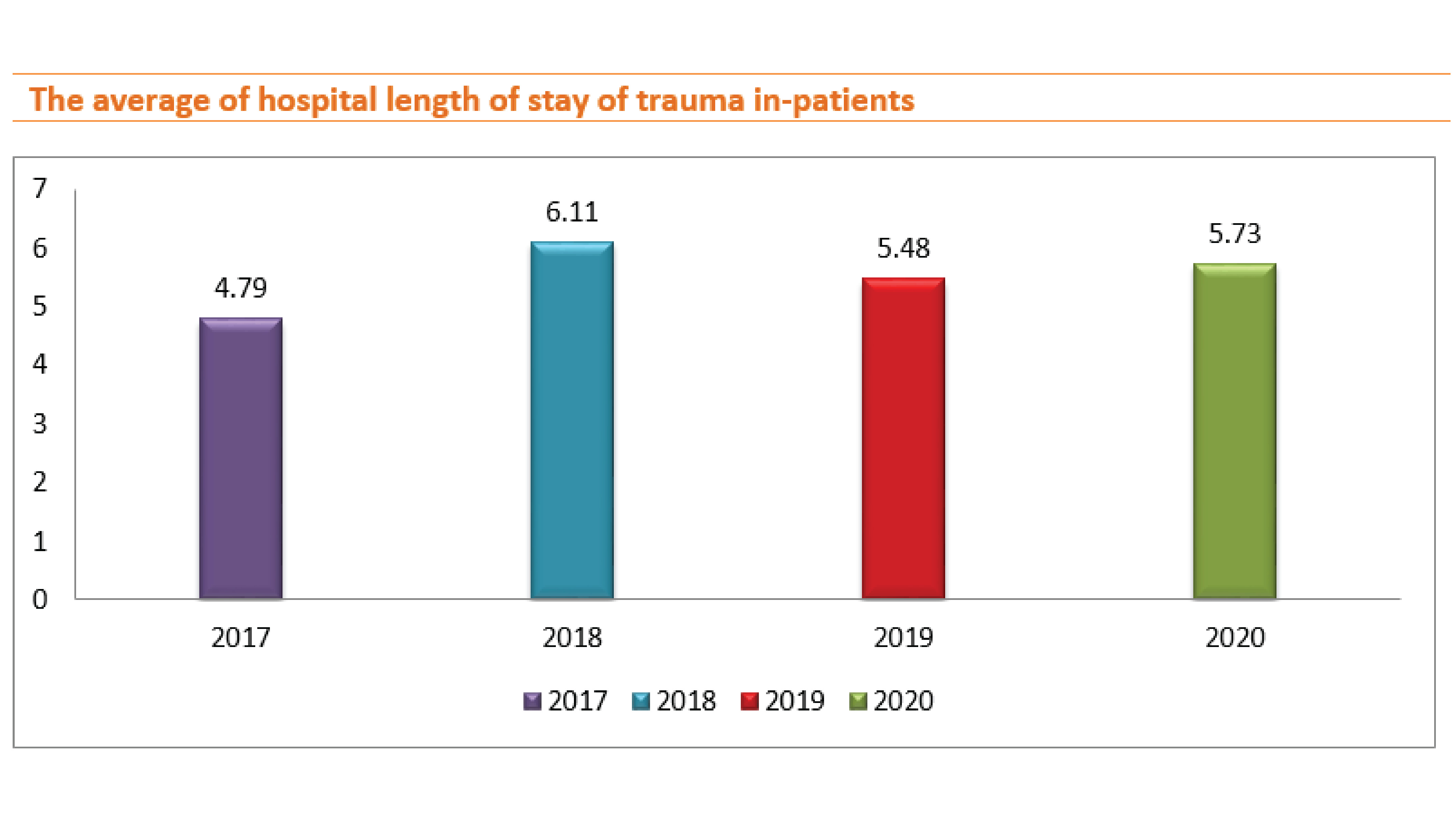
The average length of stay was changed as follows: 4.79, 6.11, 5.48, and 5.73 days in 2017, 2018, 2019, and 2020 respectively.
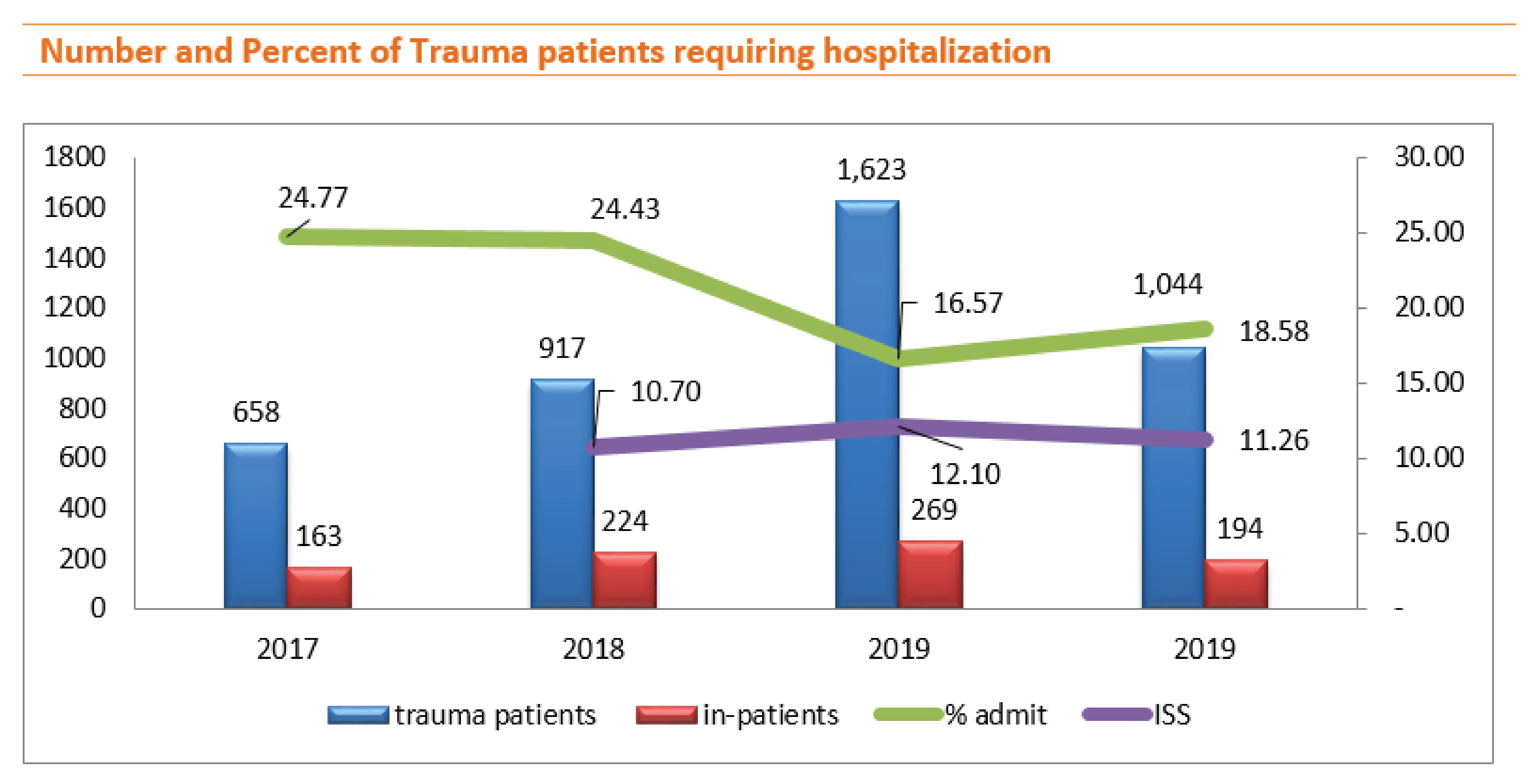
Although in 2019 the number of trauma patients was a large higher than in 2018 and the ISS was higher but on the other hand, the number of inpatients decreased. In 2020, the number of trauma patients decreased and the ISS was lower than in 2019, but the inpatient rate was higher, we found that the most important factor affecting being inpatient was the ability to pay for medical expenses.
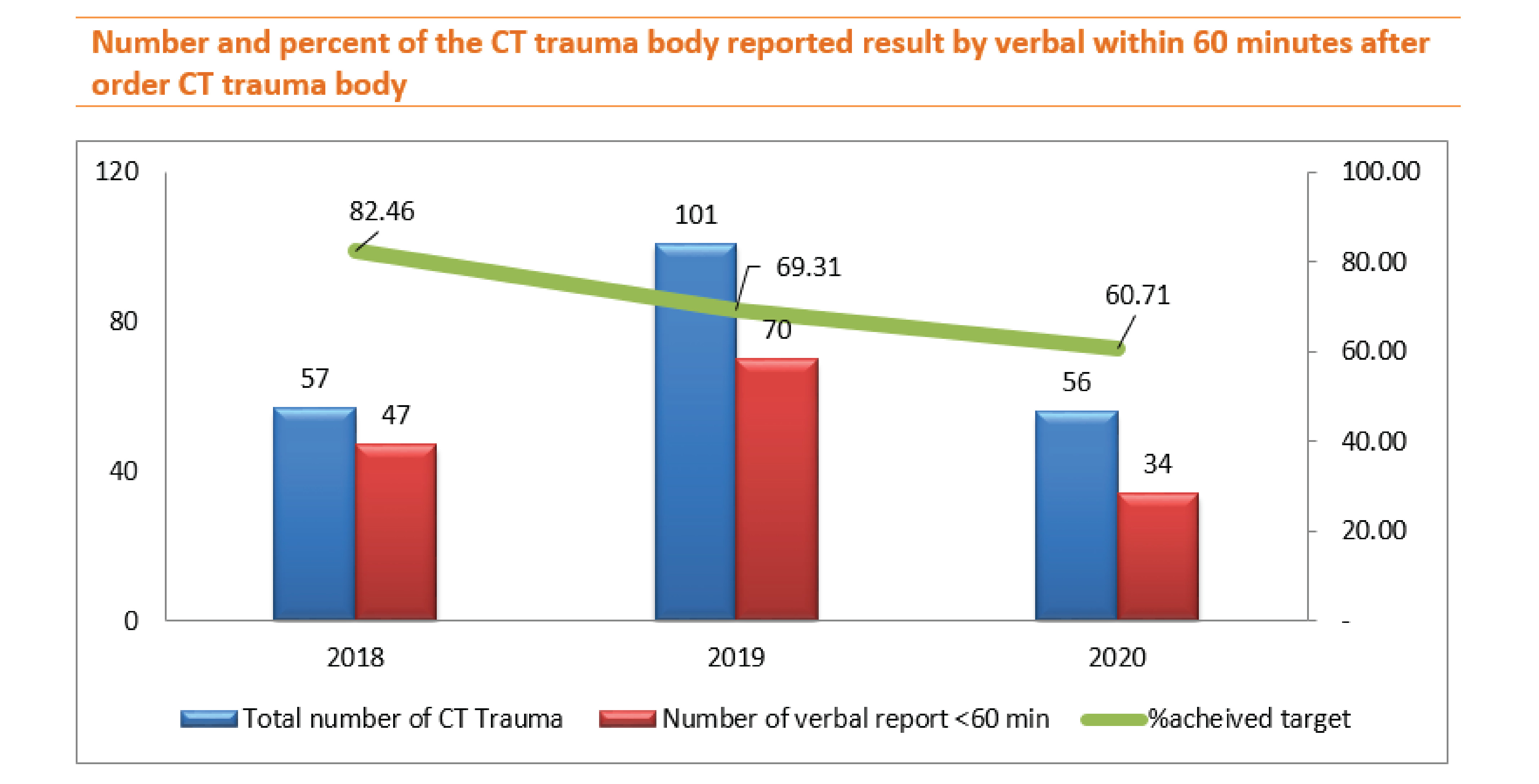
Practically, when the trauma team was alerted, they visited the patient at the emergency department and follows the patient into the CT control room to see the CT pictures by themselves and discussed treatment plans at that time. However, the data collection would record the doctor's ordered CT time to the radiologist reported by verbal time as well.
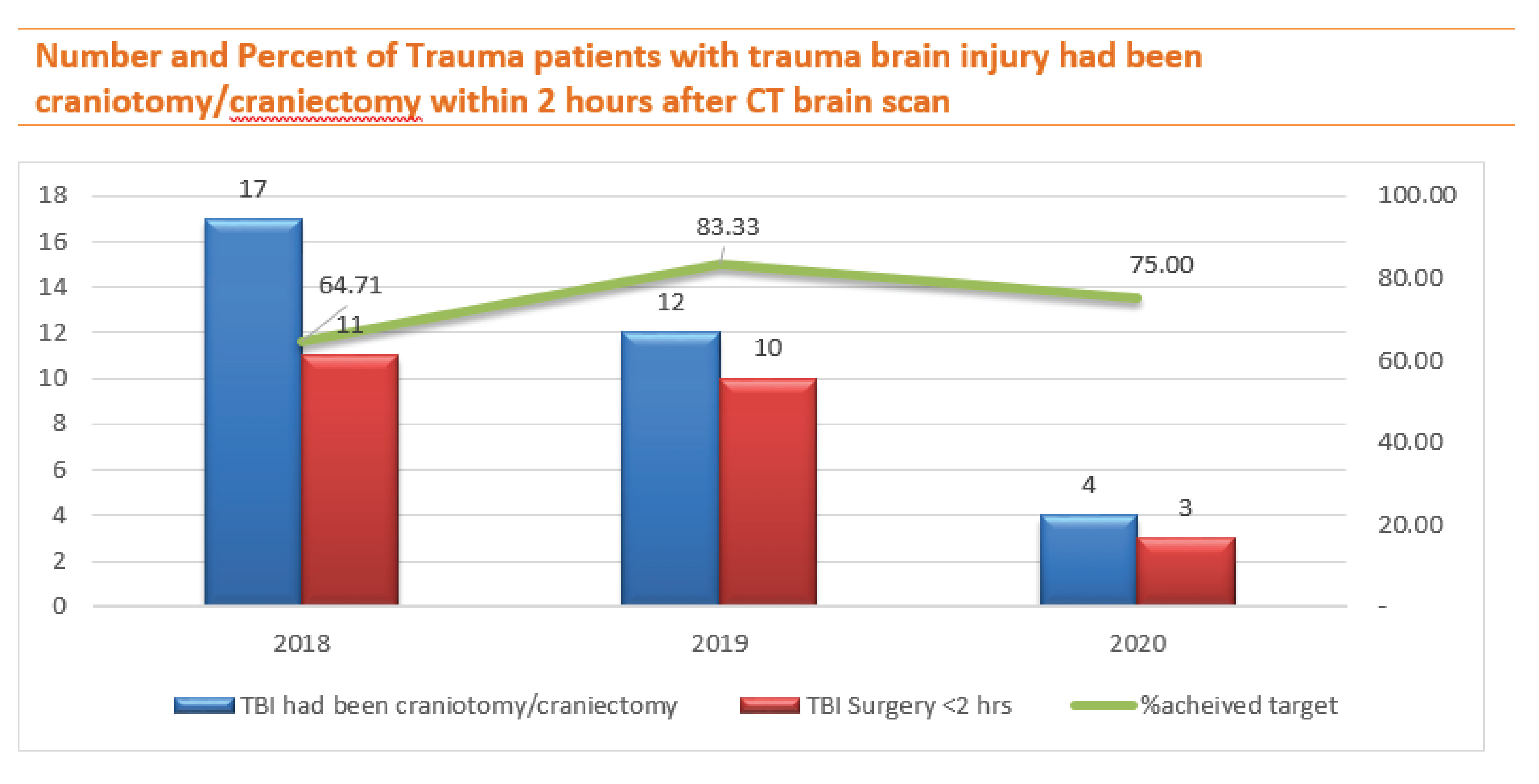
The number of TBI patients who met the criteria for craniotomy/craniectomy decreased in 2019 and 2020 gradually however, the percent of these patients sent to surgery within 2 hours declined in 2020, the reason for the delay was due to the patients’ relatives took time for discussing each other. Ten out of eleven traumatic brain injury patients had surgery more than two hours after sending a CT scan and one died due to secondary brain damage before arrival.
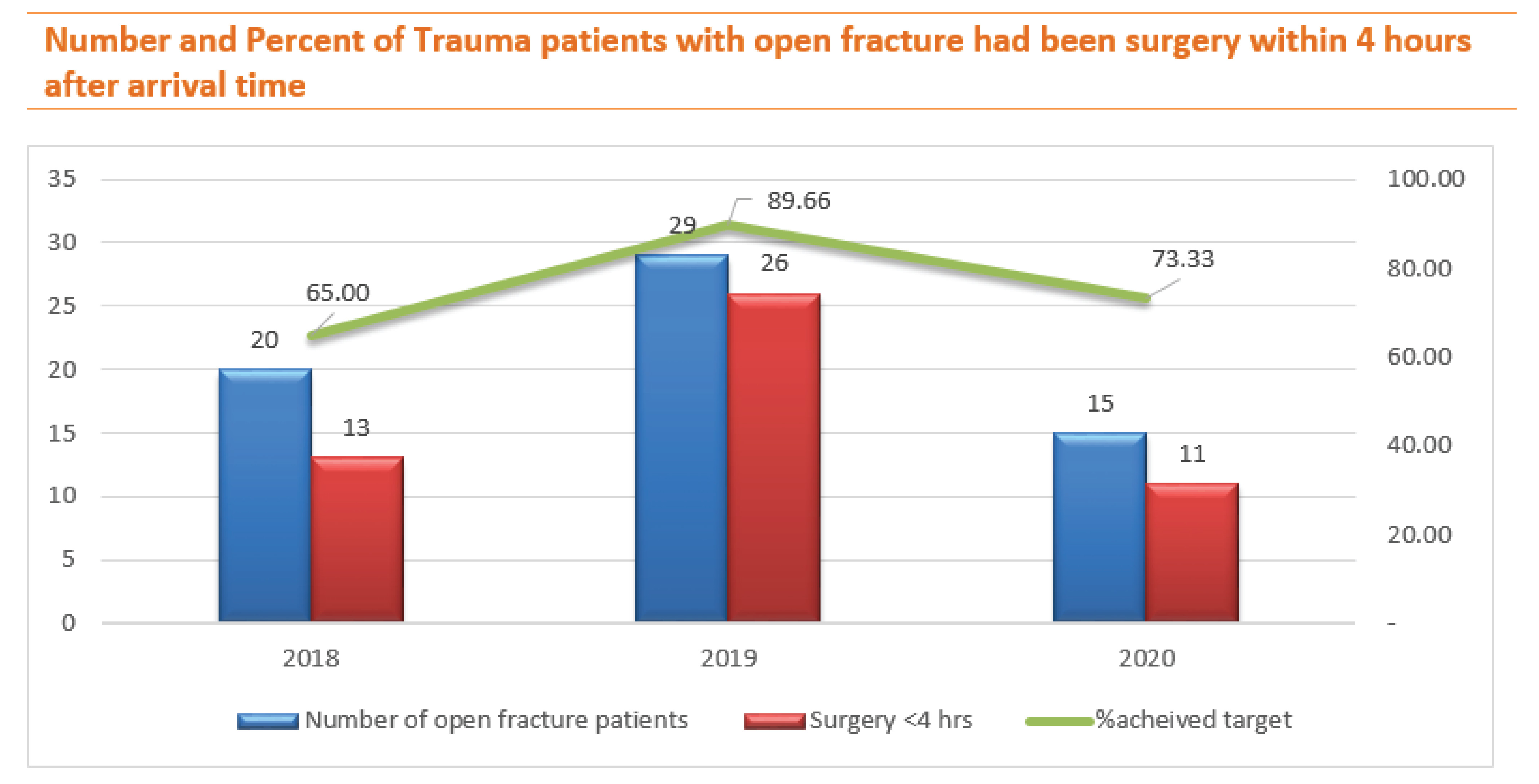
Although the number of open fracture patients increased in 2019, the percentage of surgery performed within 4 hours increased, converse to 2020 while the number of patients declined and the percentage of surgery within 4 hours also decreased, too. However, while waiting for relatives to decide to agree to surgery, orthopedics washout open wounds at the emergency department to reduce the rate of infection and all of them discharged without any infection complication.
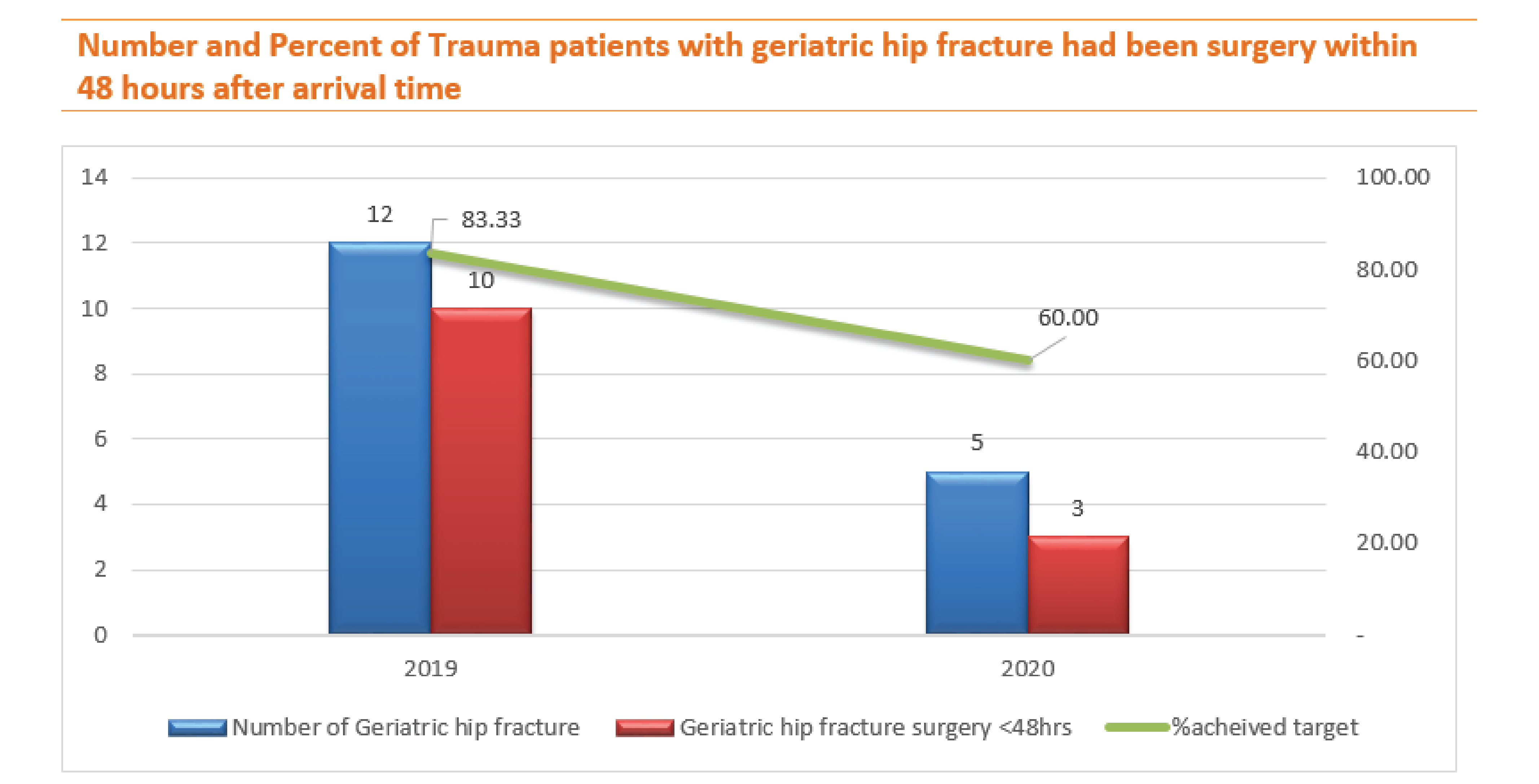
In 2020, the number of geriatric hip fracture patients greatly dropped, but the surgery rate within 48 hours dropped, too. The reason for the delayed surgery because the pandemic of COVID 19 affected the delay in the orthopedic implant importing however, all of them discharged without any complication.
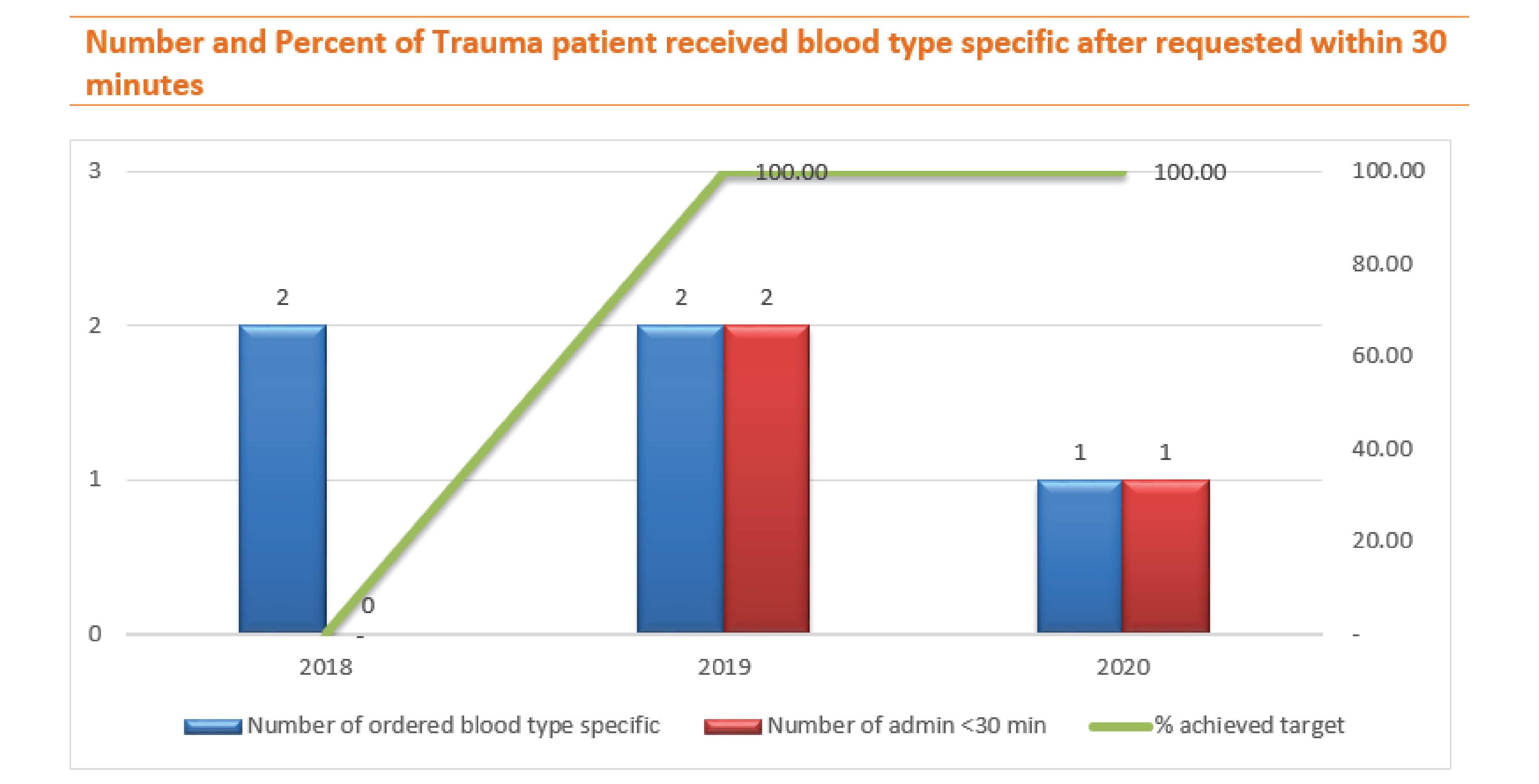
In 2018, we couldn't administration blood type-specific after requested within 30 minutes to the trauma patients at the emergency department, therefore we have to resolve those barriers together with the blood bank and emergency team, after that we were able to achieve the target in 2019 and 2020.
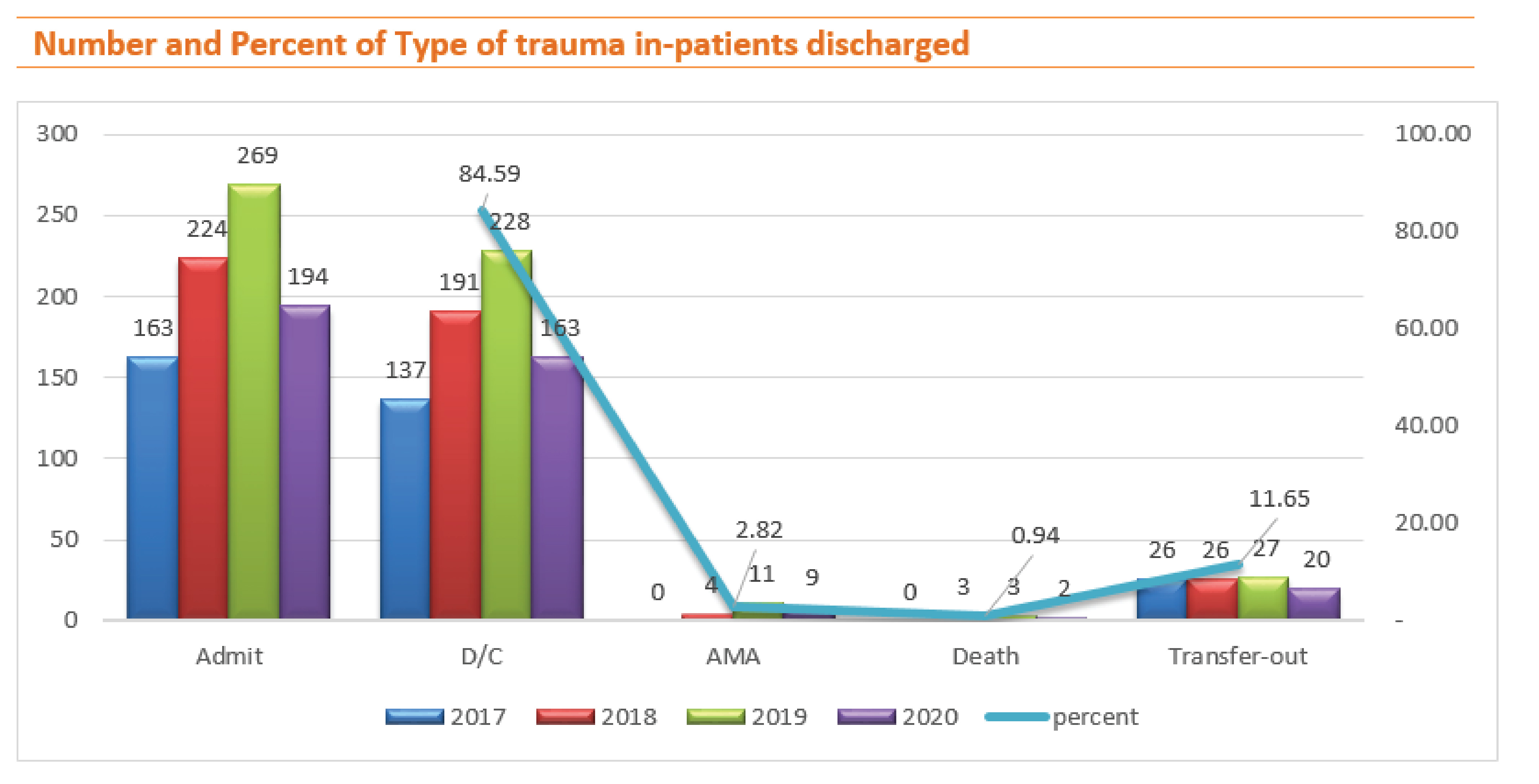
In the overview of trauma in-patient discharge type in 2017-2020, the total number of trauma4,242 and in-patient 850; discharge to home 719 (84.59%), against medical advice (AMA) 24 (2.82%), transferred out to another hospital due to finance issue 99 (11.65%), death at emergency room 3 (0.07%) and inpatient died 5 (0.59%).
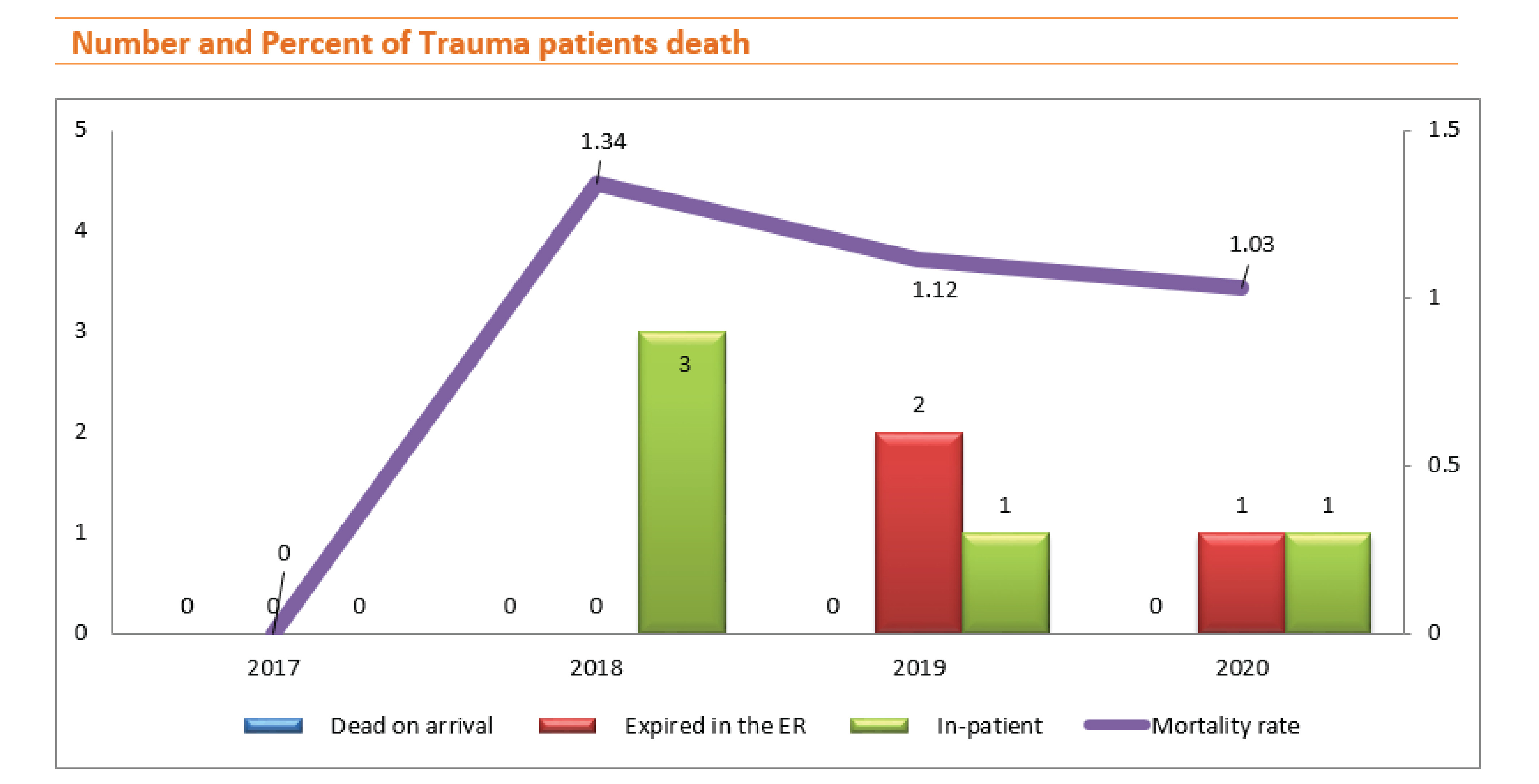
In 2017, the number of trauma patients who died was zero. The number of deaths in 2018 was 3 in-patients. In 2019, the number of deaths was 3; 2 deaths at the emergency department and 1 in-patient died. In 2020, 1 death at the emergency department and 1 in-patient died. The mortality rate was 1.34%, 1.12%, and 1.03% in 2018, 2019, and 2020 respectively.
The cause of injury of 3 deaths in 2018 was 1) traffic accident causing traumatic liver injury grade IV-V, 2) traffic accident causing severe traumatic brain injury, and 3) assaulted by the thief hit his head causing severe traumatic brain injury with secondary brain damage before arrival.
In 2019, the cause of injury of 3 deaths was 1) the patient death at Emergency Department was a traffic accident causing severe traumatic brain injury 2) the patient death at Emergency Department was falling down from height 12 meters causing severe traumatic brain injury and multiple injuries 3) the in-patient death was fallen down from height 6 meters causing severe traumatic brain injury and multiple ribs fracture.
In 2020, Total trauma patient deaths were 2, 1) 1 death at Emergency Department, the cause of injury was overlapped by a huge and heavy metal electrical gate, and 2) causes of injury of trauma in-patient death was fallen down from height >6 meters causing severe traumatic brain injury.
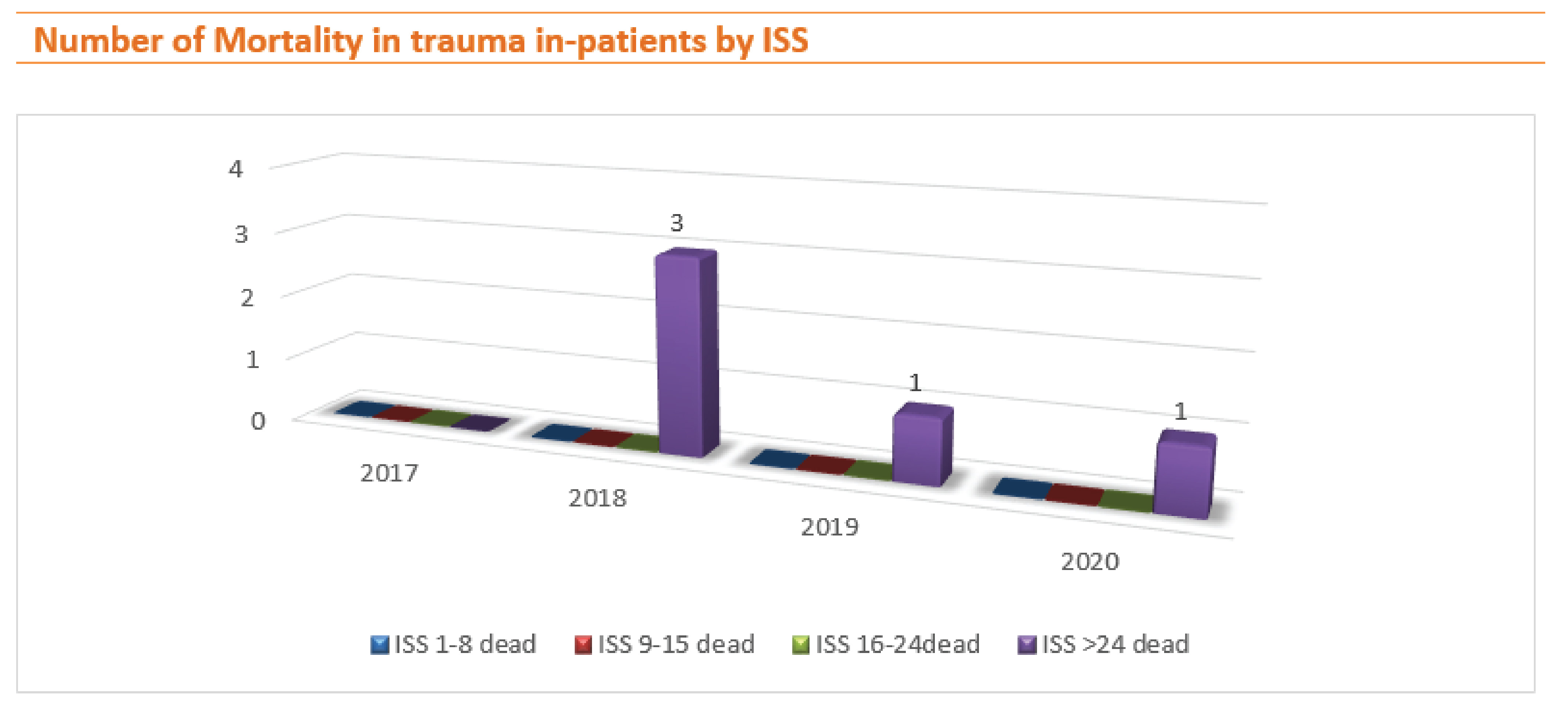
In 2018, 3 of 20 of ISS >24 death (15.00%). In 2019, 1 of 35 of ISS >24 death (2.86%), and in 2020, 1 of 17 ISS >24 deaths (5.88%).

1. BDMS COE Trauma Monthly Tele-conference
1.1 BDMS group 1 Monthly quality monitoring
1.2 Tele BDMS trauma network group 1 meeting

2. RPH code 3 drill (Mass casualty)
3. RPH code 6 drill (Fall from Height)

4. RPH trauma team meeting

5. One Hospital, Two Locations
We always training and tele-consultation between Royal Angkor International hospital and Royal Phnom Penh hospital.

6. Emergency Physician taught emergency nurses about trauma alert checklist
7. Training BLS for alliance clinics

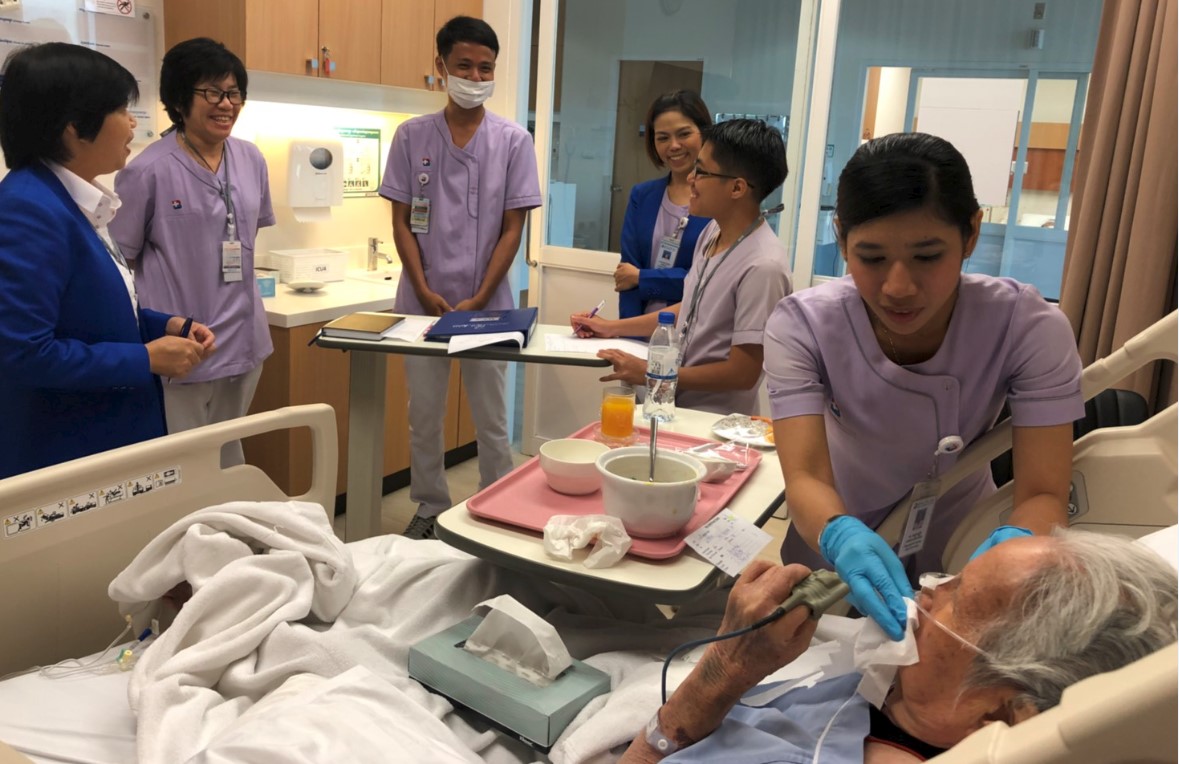
8. Nursing rounding for Geriatric hip fracture patient care in ICU
9. On the job training for new mobile ventilator by BME officer

10. JCI reaccreditation in 2020

11. Intensive Course for BDMS Trauma Nurse Coordinator Tele-conference
6 August – 3 December 2020, Mr. Wattanapong Wongbida
12. Trauma Course for Nurse Tele-conference
28 May – 24 December 2020, Mr. Wattanapong Wongbida